no doctors on callyellow3x2
In 2012, private out-of-hours provider Serco found itself in the headlines after a whistleblower revealed the company only had one GP covering a population of 500,000 people in Cornwall.1 This led to a huge controversy, with the provider being removed and an investigation by Government auditors finding 60% of providers ran shifts without the optimum staffing levels.2
Four years on a Pulse investigation has found little improvement. In fact, staffing in out-of-hours has reached ‘safety critical’ with around one in 10 providers admitting to periods with no overnight GP cover, affecting some four million people.
GP out-of-hours leaders say this is part of a ‘worrying trend’, with fewer clinicians available and services often relying on non-medically qualified urgent health practitioners, nurses and paramedics. Such staff shortages have forced some providers to shut down provision, piling pressure on other services, such as GP practices and A&E departments.
National Quality Standards3 state commissioners should ensure all patients can access a GP face to face if necessary. But a Pulse request under the Freedom of Information Act, answered by 104 out-of-hours commissioners across the UK, found 10 areas where patients were left with no GP available during out-of-hours shifts in 2016.
In Peterborough, there were nine shifts where 230,000 patients were left without access to an out-of-hours GP and all children under the age of four were ‘defaulted’ to A&E. Tower Hamlets, east London, had no GP available on 12 occasions last year. This meant a population of more than 250,000 was told to contact A&E or the ‘community night team’ for help.
In Doncaster, a lack of GPs meant nurses and upskilled paramedics were covering a population of 300,000 patients on three occasions, with no GP even available by phone on one occasion. Doncaster LMC medical secretary Dr Dean Eggitt said at the time ‘the system is not safe’, adding: ‘I think 24 hours a day patients should be able to contact a senior clinician, a GP. If that is not available that is a very serious situation that must be remedied ASAP.’
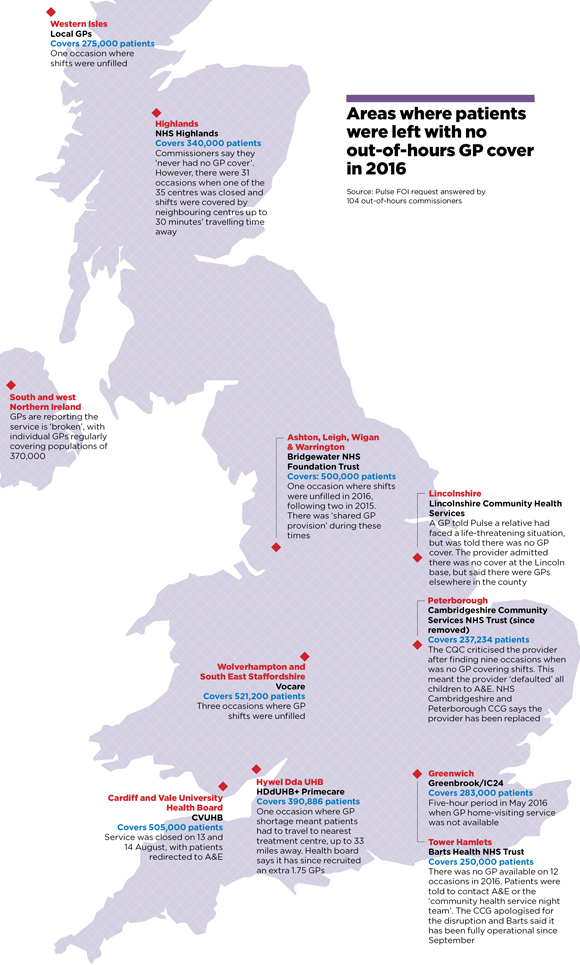
map p8 cover story580x965
PLEASE NOTE: The population covered by Western Isles out-of-hours is 27,500, not 275,000 as listed on this map. This error does not impact totals listed in the rest of the article.
UK-wide problems
The problem is not confined to England. In the Highlands, which has a population of 340,000, there were 31 occasions when one of the centres was closed due to lack of staff, with shifts covered by centres up to 30 minutes’ drive away.
In south and west Northern Ireland, individual GPs regularly have to cover populations of 370,000 overnight. Southern LMC chair Dr Frances O’Hagan, who works for the out-of-hours service, says it is ‘broken’. She adds: ‘Having only one doctor on call used to be rare but is becoming the norm.’
The CQC – which polices the safety of out-of-hours services – says it will ‘review’ the results of Pulse’s investigation. A spokesperson said: ‘We want to be confident these providers are monitoring their services effectively so patients receive safe care at all times.’
The 2012 National Audit Office report listed three causes for the reduced pool of out-of-hours GPs: in-hours workload, indemnity costs and other employment opportunities.2 If anything, four years later, these factors are even worse.
Recruitment problems in GP practices mean more locums are needed for core hours and out-of-hours providers have struggled to compete with the Government’s seven-day GP access pilots, which have offered GPs better rates and less antisocial hours.4
Having only one doctor on call used to be rare but is becoming the norm
Southern LMC chair Dr Frances O’Hagan
Dr Peter Holden, a GP in Derbyshire and a former GPC lead on urgent care, says while working for an ambulance trust he observed shifts ‘covering a very large rural patch, where there was no doctor cover’. He adds: ‘I don’t want to name them, but it’s a well-respected, well-organised, well-paying organisation. If they’re struggling, god help the others.’
Spiralling indemnity costs are a critical factor. South-east London GP Dr Emma Rowley-Conwy, an out-of-hours GP and former chair of the SELDOC out-of-hours co-operative, says: ‘We are definitely really struggling to fill our rota; we have seen a huge shift to use of locum agencies, up from 5% to nearly 40%.’
She adds: ‘Indemnity is a deterrent as it costs about £10 an hour to get insurance from a defence organisation.’
NHS England has offered to pay for ‘additional shifts’ taken on by GPs out of hours over winter, and claims 500 GPs took advantage of this to provide 15,000 additional shifts last year. But Dr Rowley-Conwy says this wasn’t the feeling on the ground: ‘We had no GPs who managed to get any indemnity back under the scheme. The criteria were impossible to meet.’ As a result, SELDOC had to invest £500,000 in an indemnity scheme in a bid to attract GPs.
But Dr John O’Malley, medical director of Stockport out-of-hours provider Mastercall, tells Pulse the biggest factor is a more ‘fundamental change in attitudes and lifestyles’.
‘For old fogeys like me on-call was part of the territory,’ he says. ‘But I’ve been wrong all these years, worklife balance is a perfectly good ambition. That’s why many [younger] doctors aren’t doing out of hours.’
All this comes as demand continues to grow. A survey by Urgent Health UK – which represents out-of-hours providers – of 12 of its member organisations found an estimated 11% to 15% increase in demand over last winter.
Dr O’Malley says: ‘A lot of the stuff we pick up on could be done in the daytime if we had enough bloody GPs in this country.’
And emergency care services find themselves treating more people unable to get out-of-hours GP care and GP practices have to deal with more paperwork and more patients requiring emergency appointments in the morning.
As Essex LMC chair Dr Brian Balmer says: ‘Patients ask for more early appointments when the out-of-hours service is struggling, or will flood to A&E.’
For Dr Fay Wilson, CEO and group medical director of the BADGER Group out-of-hours GP co-op in the West Midlands, the problem is ‘NHS England doesn’t understand GP out of hours’.
‘Over the holidays we’ve dealt with thousands upon thousands of people. If they’d all had to go to A&E, the health system would have collapsed. And yet they forget about us, they kind of airbrush us out of the story,’ she says.
Provider view: ‘It is a worrying trend’

dr abrams simon neil o’connor 330×330
Just as in many areas of the NHS, we are seeing a downgrading of services – shorter opening hours, longer distances to travel and fewer clinicians available. It is a worrying trend.
I talk with many medical directors and CEOs of out-of-hours providers. In the past year they have repeatedly referred to difficulties filling shifts, notably with GPs; it can be a last-minute appointment that keeps the service afloat, especially at weekends. Additional funding can be required to attract takers and even then there are occasions when rotas are not full.
Then, closing urgent care centres or staggering opening times is the only option. This probably impacts more on rural communities where patients are already travelling several miles to see a GP out of hours.
The solutions are a sustained resolution of the indemnity problem, recognition that good out-of-hours providers are a cost-effective way of keeping people out of hospital, and adequate funding. Resources have not kept up with costs: CQC requirements, leasing equipment and IT are all costing more but contract prices are fixed.
Erosion of these services not only raises clinical risk in the community but adds to pressure on A&E.
Dr Simon Abrams is a GP in Everton and chair of Urgent Health UK
References
1 GPs left to cover 500,000 patients alone out of hours. The Guardian, 2012. tinyurl.com/guardian-500k
2 National Audit Office. Out-of-Hours GP Services in England, Sept 2014. tinyurl.com/OOH-NAO
3 Out-of-hours services: a commissioning handbook. 2012. tinyurl.com/OOH-handbook
4 ‘Seven-day GP access scheme causes “mayhem” in out-of-hours workforce’. Pulse, 2015. tinyurl.com/pulse-mayhem
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













