Pulse summarises April’s talking points: What happens when fit note responsibility is taken away from GPs, and what will happen with the RCGP consultation on PAs
What does the removal of sick notes mean for GPs?
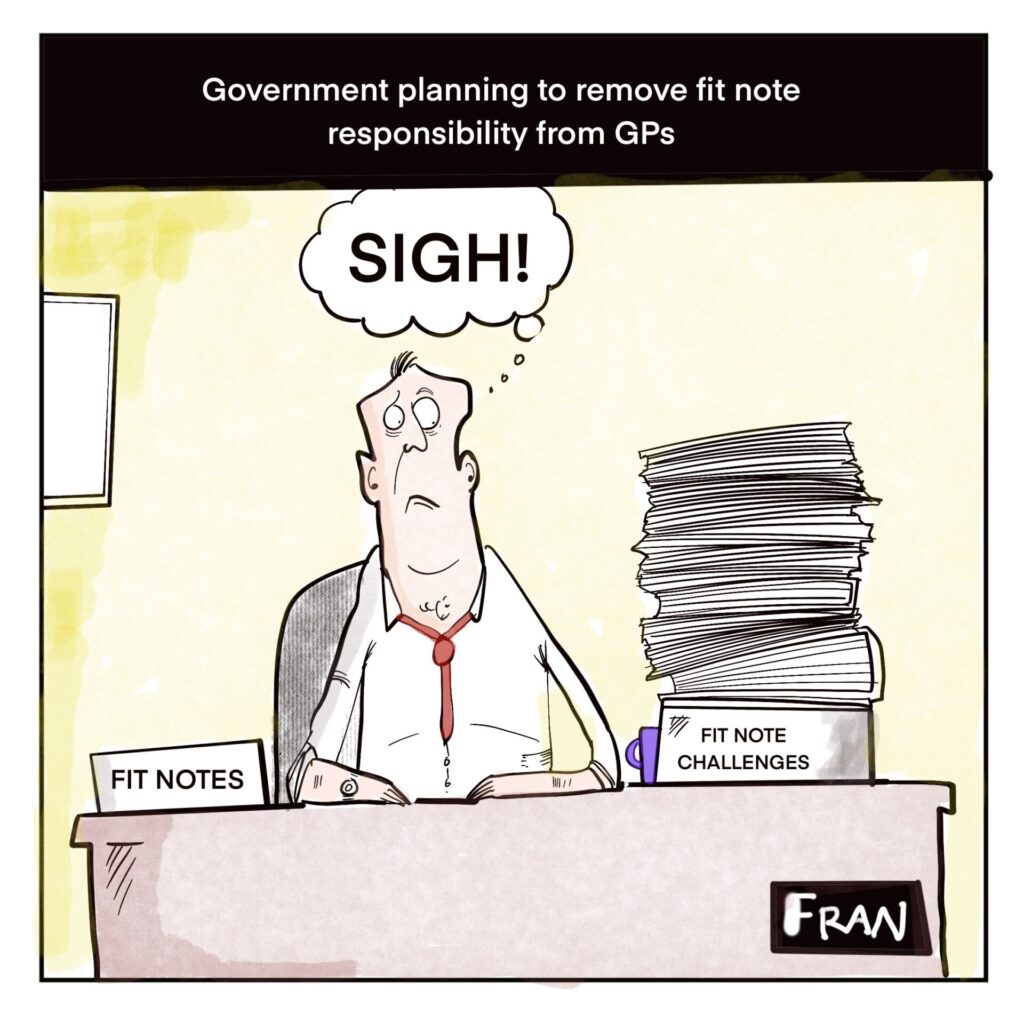
Rishi Sunak’s speech on welfare reforms earlier this month saw him set out plans to address the ‘sick note culture’ in the UK. His idea? Removing the responsibility of signing off fit notes from GPs and giving it to other health professionals and specialists.
This is not the first time that the Med 3 system has been re-worked to reduce GP workload. In 2021 the Government allowed for fit notes to be issued digitally rather than in paper and pen. The following year, legislation was brought in to allow a wider range of healthcare professionals to sign Med 3s – not just GPs.
And now it seems we are taking it one step further: no fit notes to be issued by GPs at all. Sunak’s decision makes no reference to the GP crisis, and instead seems to stem from his concern about patients exploiting the welfare system, and ‘taking advantage of the hardworking taxpayers who fund it.’ Regardless of his intention though, the plans have been met with a mixed reception. BMA GP Committee England chair Dr Katie Bramall-Stainer said that whilst a review of the fit note system could relieve GPs’ administrative burden, the Prime Minister should instead focus his efforts on other issues, such as long hospital waiting lists and removing the barriers that stop patients from receiving the physical and mental healthcare they need in the first place.
As also pointed out by Copperfield, the reduction of admin work that comes with this measure will be welcomed by GPs. In an already time-squeezed profession, not having to judge an individual’s ability to work could free up valuable appointment slots for other patients, as well as giving GPs to complete other admin tasks. And it is hard to argue with that, especially when doctors are inclined to side with their patient’s fit note requests lest they find themselves damaging the relationship with the patient, or facing formal complaint.
It is unlikely that there will be a clean and immediate separation between GPs and fit notes – especially given that there is no further detail on what the future Med 3 process might look like. At present, we have been told that fit note responsibility will be given to specialist work and health professionals who have the dedicated time to provide an objective assessment of someone’s ability to work.
First off, how will these independent specialists access individual patients’ history when trying to access their ability to work? Of course they will have a discussion with the patient themself, but will that be all there is to it? There will likely have to be some degree of interaction with a GP to provide notes to allow a fitness-to-work consultation to take place. The back and forth between parties might mean that GPs spend an equivalent – or perhaps greater – amount of time dealing with fit notes than they currently do.
Sunak said that GPs were signing people off as ill too easily, with only 6% of all fit notes designating patients as ‘maybe fit for work.’ Part of the decision to relocate the responsibility is to increase this percentage and have more people working. We can expect many patients who will be signed off as ‘fit to work’ – when a GP might have instead declared them as sick – to (understandably) try to contest the situation, and write to their doctor for a reference. If this becomes the case, dealing with appeals against the independent fitness consultations might mean GPs still end up doing a great deal of heavy lifting to advocate for their patients.
In the same vein, trying to communicate to patients who are used to a GP fit note system that this is no longer the case will likely be an uphill battle. Old habits die hard and trying to explain to patients that they can no longer request a fit note from their GP is sure to: A) take a few rounds of explaining and; B) rattle some cages.
Some may argue that the stripping of sick note responsibility diminishes the role of a GP and weakens the strong doctor/patient relationship that primary care can be used to harness. However, it seems unlikely that any changes to the system will cut out GPs instantaneously and completely any time soon.

What is the Royal College going to do about PAs?
Another month, another consultation on physician associates. So far this year we have already had one from NHS England about the career framework of PAs, and another from the GMC about how the role should be regulated. Now comes the long-awaited turn of the Royal College of GPs. RCGP chair Professor Kamila Hawthorne has described the consultation as an opportunity to learn how best to ‘protect patients, physician associates themselves, as well as GPs and their existing staff.’
This comes after months of confusion and indecisiveness regarding the RCGP’s stance on PAs. In February, BMA GPC chair Dr Katie Bramall-Stainer (in a now deleted post on X) accused Professor Hawthorne of not being transparent about her involvement in designing and developing a postgraduate course for PAs at the University of Surrey. Later that month, the college had to remove a 2017 case study detailing the work and supervision arrangements of a PA in general practice after it attracted criticism and claims of inaccuracies from doctors. And only last month, the RCGP changed its stance on PAs, adding more ‘red lines’ and voting against the GMC to regulate the new role.
Some feel like this consultation is a bit ‘too little, too late’ – particularly on that final point. The legislation bringing the PA role under GMC regulation has already passed through the House of Lords, and will come into effect before the end of the year. Having PAs under GMC remit will almost definitely cause much more confusion for patients about the differences between doctors and PAs. Professor Hawthorne further commented that because the legislation had gone through, the RCGP will ‘need to enter into discussion with the GMC and other stakeholders to look at how these concerns can be addressed.’
With that in mind and assuming that divorcing PA regulation from the GMC is impossible at this point, the RCGP is asking GPs as part of the consultation, what prefix should be used for a PA’s GMC number to differentiate it from that of a doctor’s. The current options stand as: an ‘A’ (the GMC’s proposal); ‘PA’; ‘MAP’ or other. This does little to quell the issue of differentiating PAs from doctors: sure the GMC number will be ever so slightly different, but that will ultimately mean nothing to the patient in front of them. If ensuring that the patients are clear on the title and role of their clinician is a priority, then this still falls far too short.
One of the new ‘red lines’ introduced by the RCGP in March focuses on workforce concerns: funding and learning resources within general practice must be prioritised for training and retaining GPs. However, a Pulse exclusive revealed that a number of primary care recruitment agencies are telling practices to hire PAs and other ARRS staff instead of locum GPs as a ‘cost-effective alternative.’ Bearing such stories in mind, it is hard to see how the college will be able to effectively advocate for the prioritisation of GPs to the GMC.
In fairness to the college, the consultation is providing a platform for GPs to have an influential say on the PA discussion. The consultation asks GPs to share their experiences of working with PAs (if applicable), as well as gathering opinion on what should be in place for PAs working in primary care. This includes training, supervision, CPD, triage systems and more. By using the case-based answers from that, there will hopefully be substantial data to forge an argument for tight and effective regulation of the PA role.
For anyone who has yet to trudge through the 40+ question consultation, we’ll leave you with a tempting moment of comedy to spur you on to complete it. When asked about the benefits (if any) you consider there to be with the PA role in general practice, there are only six options (including an ‘other’ option and a ‘none’.) The following question – what challenges (if any) do you see – provides a bountiful 14 options to pick and mix from.
It’s the small things in life…
















Medical Royal Colleges should be championing ‘Evidence Based Medicine’, yet there seems to be a dearth of evidence for or against PAs, due to lack of research studies and quality data. there is also a shortage of ‘low-grade’ evidence (types C-E), with strong views on both sides very recently, but poor concordance over time.
It is like an unknown drug company buying some high-profile Ad. space or an ‘influencer’ to sell massive quantities of a drug nobody has ever thought about before, as a panacea for all ills preferable to all established therapies, and only applying for a marketting authorisation after selling the first 3 million doses, and without record of the clinical trials (if there were any) ! That drug may be extremely useful for certain conditions, but it’s reputation could be harmed forever by bad marketing and regulation, but by then the inventor will have made their profit and run away from the fallout.
Freeing up time to allow GP’s
Freeing up time to allow GP’s time to do other tasks. How about freeing up time so we do less work for free.
If asked about fitness just remember you are not OH trained and so can’t comment and are not insured. When it comes to simple list of problems remember all patients have access to their medical
Information on NHS App so refer person to the patients NHS App which the patient can share.