Hold your nose! NICE’s asthma guidance is here

NICE’s new guideline on asthma has been widely derided by experts, despite being delayed for two years for extensive piloting.
Click here to download
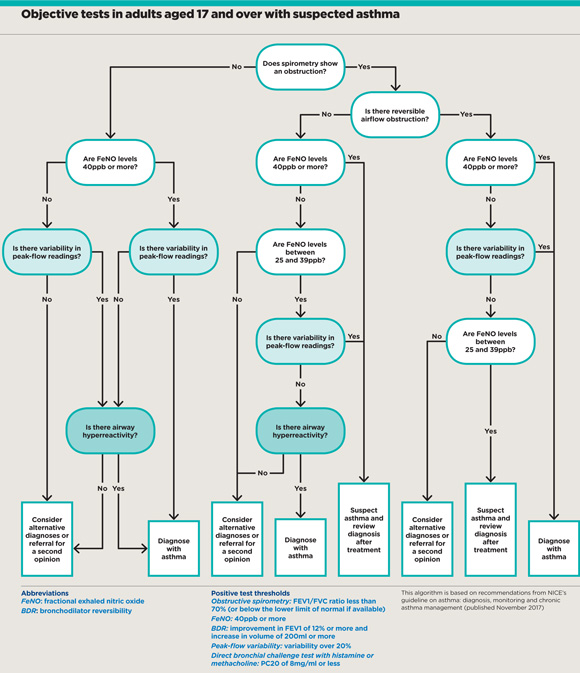
Under the new recommendations, GPs are expected to carry out objective testing to confirm a diagnosis of asthma, including spirometry, and forced exhaled nitric oxide (FeNO) and bronchial challenge testing, alongside a clinical assessment of symptoms.
NICE’s approach contradicts the gold-standard BTS/SIGN recommendations, which state GPs can confirm a diagnosis based on a trial of treatment in patients whose symptoms strongly suggest asthma.
It claims its advice will make diagnosis more accurate and treatment more effective. When the institute first released the guideline in 2015, it claimed 30% of patients diagnosed with asthma – more than one million people – might not actually have the disease.
NICE also recommends adding a leukotriene receptor antagonist (LTRA) tablet to inhaled corticosteroid treatment before trying a long-acting β-agonist (LABA), as they are cheaper and therefore more cost effective. In contrast, BTS/SIGN urges GPs to offer a LABA as a first-line add-on therapy for patients whose asthma is not controlled on inhaled corticosteroids alone.
‘There isn’t access to these resources’
Dr Dermot Ryan
NICE’s recommendations have faced huge criticism from all sections of the profession since they were first released for consultation in 2015. At the time, the RCGP and BMA pointed out the new diagnostic tests were too costly to be carried out in primary care, and that asking GPs to adhere to the new treatment algorithm would increase appointments, referrals and costs.

c0327295 spirometry spl
As a result, NICE took the unprecedented step of delaying publication of the guideline in September 2015. It carried out pilot studies to test their feasibility and launched a fresh consultation last year even though GPs in the pilot areas said the new objective tests were time-consuming and did not necessarily improve diagnostic accuracy.
Diagnostic hubs
But GPs’ concerns have not been heeded, although the final guideline does concede the recommendations will take ‘some time to implement, with additional infrastructure and training needed in primary care’, and urges GPs to ‘implement what they can’.
NICE says developing new ‘diagnostic hubs’ could make testing efficient and affordable, and could save approximately £12m per year in England.
But Dr Dermot Ryan, GP and president of the Respiratory Effectiveness Group, says GPs have been left in a precarious position. ‘Most GPs don’t have access to FeNO and most CCGs don’t have the funds or the know-how.
‘Furthermore, many adults with asthma don’t have a phenotype that leads to elevated FeNO results, so a negative FeNO doesn’t mean they haven’t got asthma. I think the guideline is setting GPs up for failure because there isn’t access to these resources.’
The BMA response to the guideline says it is essential diagnostic hubs are established to ‘provide a full respiratory testing service to cover all aspects of the diagnostic process’, but warns: ‘In many areas GPs are carrying out this work without appropriate resources.’
NICE’s direct contradiction of the established BTS/SIGN recommendations has also been criticised for the potential to cause ‘confusion’.
Primary Care Respiratory Society policy lead Dr Duncan Keeley says the PCRS ‘advised against’ the guideline’s publication’, adding: ‘We are concerned at the potential for confusion among health professionals caused by conflicting guideline advice… We would encourage NICE and BTS/SIGN to cooperate on a single guideline in future.’
The recommendations on asthma management have attracted similar controversy. NICE claims they could save an estimated £2m a year for every 10,000 people who take up LRTAs. Dr John Alexander, consultant in paediatric intensive care at University Hospitals of North Midlands NHS Trust and co-chair of the guideline committee, said: ‘This sets out the most effective options to treat asthma to make patients feel better and potentially save the NHS money.’
Worse outcomes
But GPs fear patients may neglect their inhalers in favour of taking LTRAs, leading to poorer outcomes.

dr mark levy 330x330px
Dr Mark Levy, clinical lead for the National Review of Asthma Deaths and a respiratory GPSI in north London, warns patient deaths may even result: ‘I cannot understand why we’re going against current international guidance. Nobody can know the long-term effect, but the logical conclusion is admissions will go up and deaths will go up as well.’
Dr Ryan says this is simply being done for ‘cost minimisation’, and that European colleagues will be ‘laughing’ at England, while Scottish practices – to whom the guideline does not apply – ‘will look down their noses in scorn at this outlandish proposal’.
He adds: ‘In the best trials, there are only a few people who respond well to LTRAs. The rest are coming back four to eight weeks after being given the LTRA, during which time they have symptoms and may have an exacerbation.’
This has workload implications, Dr Ryan warns: ‘Practices have to provide another appointment and the patient is following a confusing mixed regimen.’
Ultimately, however, the feeling among grassroots GPs is that the whole guideline is unrealistic for practices and patients. Family Doctor Association chair Dr Peter Swinyard says: ‘There will be a lot of people with “wheezing disease” who need inhalers – we’ll just be calling it “wheezing disease” rather than asthma.
‘It just makes me wonder where NICE’s reality check is and why they don’t realise we can’t do these things in general practice. It may be a gold standard but it’s aspirational rather than achievable.’
NICE guide to treating asthma
• Offer a short-acting ß-agonist as a reliever treatment to adults with newly diagnosed asthma.
• Offer a low dose of inhaled corticosteroid as first-line maintenance treatment to adults.
• If this does not control the asthma, offer an LTRA and review the response after four to eight weeks.
• If the asthma remains uncontrolled, add a LABA in combination with the inhaled corticosteroid.
• Monitor asthma control at every review and consider using a validated questionnaire for this in adults.
• Do not routinely use FeNO to monitor asthma control but consider FeNO measurement as an option to support asthma management in patients whose asthma remains uncontrolled despite using inhaled corticosteroids.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.