Last month, we celebrated 60 years of Pulse with a look back at the issues faced by general practice. The slightly tongue-in-cheek angle was that the issues have remained the same over the years.
When our successors look back at general practice, the chances are they will divide general practice into two eras – Before Coronavirus and After Coronavirus. This is an issue on a scale we have never seen before.
All the important issues facing general practice are suddenly small components of the only issue that matters to anyone right now. Covid-19 is already exacerbating the recruitment crisis, the biggest problem facing general practice until last month, through the number of GPs needing to self-isolate. And it has also triggered the most drastic recruitment measures we’ve seen, in the form of removing red tape for retired GPs and speeding up medical students’ graduation.
There has been a downgrading of the need for routine CQC inspections, which have been indefinitely postponed. Rationing, although indicative of the state of the NHS, has become almost irrelevant, as most elective procedures are being cancelled. And the boxes GPs need to tick to earn money – on QOF and the primary care network DES for example – have disappeared.
Already we can see the effect of Covid-19 for the medium and longer term. As Dr Peter Swinyard, former chair of the Family Doctor Association, put it: ‘I think that the nature of general practice will be changed forever by this virus.’
In the medium term – around June when cases are expected to peak – GPs will be dealing with patients who would normally be seen in secondary care. NHS England Guidance from 17 March puts this starkly: ‘Community health providers must take immediate full responsibility for urgent discharge of all eligible patients identified by acute providers on a discharge list.’
The likelihood is high that almost all non two-week-wait cancer referrals and non-urgent appointments will be cancelled in secondary care and, as a result of GPs dealing with these patients, the vast majority of GP routine appointments will have to be cancelled.
In a statement on 18 March, BMA GP Committee chair Dr Richard Vautrey said: ‘The way GPs and their teams work, both in hospitals and the community, will rapidly change following the announcement that all non-emergency operations will be temporarily cancelled in the NHS due to Covid-19.
‘I think that the nature of general practice will be changed forever by this virus.’
Dr Peter Swinyard
‘As a result, we do anticipate significantly higher pressures in an already challenged primary care system as patients turn to their family doctors to monitor their conditions while awaiting treatment.’
South-west London GP and professor of primary care at Imperial College London Professor Azeem Majeed said this will have ramifications for those with long-term conditions: ‘There are many hospital admissions from problems such as COPD, heart disease, diabetes, kidney disease and so on. If these patients are not well managed by the NHS, this will lead to poorer health outcomes for them.
‘Likewise, if patients are discharged too early, they are at risk of readmission as well as increasing GP workload.’
There are obviously major safety implications if GPs are asked to act beyond their competence. But the regulators have said this will be taken into account. Chief medical officer Professor Chris Whitty said in a letter dated 12 March that doctors ‘are expected to follow GMC guidance’, but the principles ‘rightly take account of the realities of a very abnormal emergency situation… Clinicians may need to depart, possibly significantly, from established procedures in order to care for patients in the highly challenging but time-bound circumstances of the peak of an epidemic’.
In the early weeks of the crisis, the public has been understanding. But, as West Sussex GP Dr Richard Cook put it: ‘There is a lot of goodwill out there at the moment, but this will not last.’
This will, of course, be exacerbated by the decimation of the GP workforce. The first reports suggested that 20% of the whole UK workforce could be off work at any one time as a result of the pandemic, and there have been dozens of early reports of GPs having to self-isolate.
Much will depend on the availability of testing for healthcare workers over the next few months. Birmingham GP and academic Dr Samuel Finnikin was self-isolating due to mild suspected Covid-19. He said: ‘As a result, my wife, also a GP, is not able to work for 14 days. If we could test, and I was negative, we could both go back to work sooner. If I was positive, at least we would know there is a good chance I wouldn’t need to isolate again – although advice about this is not yet clear. There will be lots of frontline staff not able to work because of household members testing positive.
‘I just want to get back to work to help ease the pressure on the system as much as I can.’
At the same time, there have been issues around protective equipment. As of the week beginning 16 March, just 15% of 550 GPs said they had received adequate equipment, while 37% said they had received some but not enough and a further 37% said they had received none. And GPs expressed concern after receiving face masks with expiry dates of 2016 that had stickers saying ‘2021’ – although the Government quickly moved to say these were ‘safe’. It later said there had been supply issues in China, meaning it could take a while for adequate supplies to come through.
‘There is a lot of goodwill out there at the moment, but this will not last’
Dr Richard Cook
The health authorities seem to understand that NHS workers are a priceless commodity. They have taken the extraordinary steps of offering healthcare workers the option of staying in NHS-reimbursed hotel accommodation while they continue to work and redeploying clinically qualified staff at NHS England/Improvement to frontline practice.
But the bigger recruitment measures surround changes to bring retired doctors back into practice. This involves the GMC contacting doctors who have retired in the past three years and suspending the need for them to revalidate. At the same time, ‘urgent work’ is under way to deploy medical and nursing students, and clinical academics.
There is an added complication for retired doctors, said Professor Majeed: ‘Like others, I have concerns that retired doctors are in a high-risk group for complications and death. They could play a role in non-direct facing clinical work such as telephone triage and supporting NHS 111.’
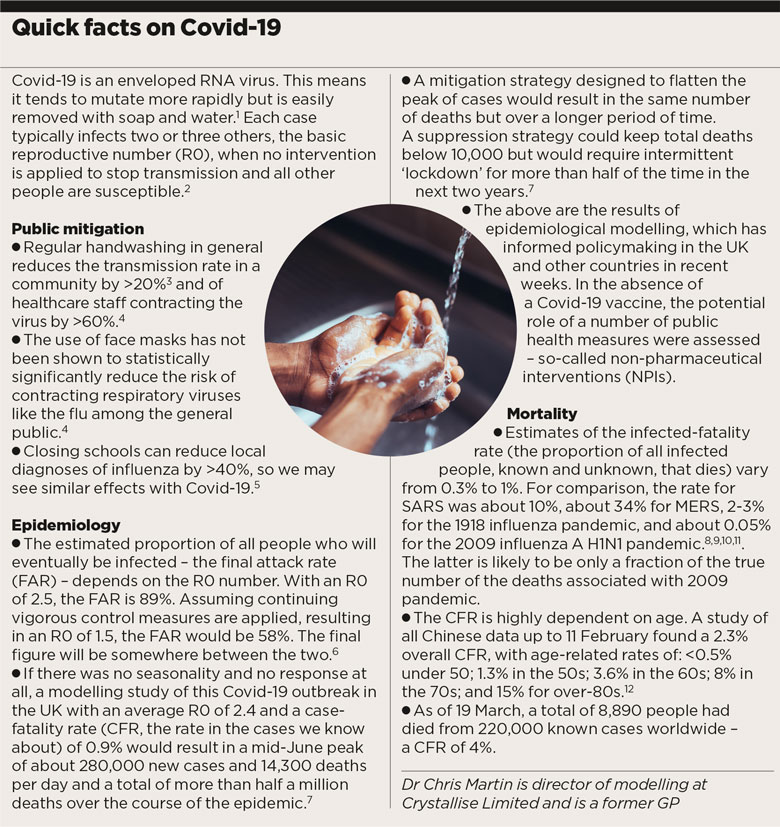
pulse quick facts on covid19 780x827px
He added: ‘Medical students can also play an important role but they should not work beyond their level of training. For example, they could carry out similar work to healthcare assistants in assessing patients. They could not though make a diagnosis, order investigations or prescribe.’
One of the major changes being brought in to combat the virus is the use of video consultations. And this is a measure that could well lead to long-term changes to general practice.
Professor Trisha Greenhalgh, professor of primary care health sciences at the University of Oxford, said: ‘What our research shows is that while until now it hasn’t been worth the hassle, suddenly that has completely changed and it is worth the hassle, because doctors are dying. Doctors are dying, patients are dying, and there is an overwhelming reason why we now need to consult remotely.’
EMIS immediately offered all 4,000 of its client practices free access to video consultations, and accuRx,a company that offers free video consultations for practices, reported 1,300 practices signing up within a day of launch on 6 March.
However, Professor Greenhalgh said: ‘What you’ve got is loads of randomised trials saying safe and acceptable, but actually they hadn’t been tested on the situation we’ve got now. Which is overwhelming demand, a deadly disease sweeping the world, people incredibly anxious and a situation where it is completely unknown what is going to happen. The research literature doesn’t help us.’
But she added: ‘As long as the video technology works you can have quite a good video consultation. The patient and the doctor or nurse seem to interact in very similar ways, and you can even do a limited physical examination, so there is quite a lot that you can do.’
GPs believe this could lead to long-term changes. Dr Benjamin Brown, senior academic GP at the University of Manchester, said: ‘I think that if anything this is a great opportunity for online consultations and video consultations, and may result in long-lasting change in the NHS towards these methods.’ BMA GP trainees subcommittee co-chair Dr Sandesh Gulhane agreed, saying: ‘It will change how we access healthcare and provide it forever.’
A potentially even greater change in the long term could be in patient behaviour. One in five GPs responding to a Pulse survey reported a decrease in patient demand in the first couple of weeks of the pandemic, although 33% said there had been little change.
Of course, 38% still saw an increase in demand but this is surprisingly low at a time of anxiety for all patients. One GP said: ‘Patients with colds seem to be staying away and some have said they don’t want to come in, can we deal with their problem without an appointment – all has been very sensible so far.’ A further change may also be more appreciation of the benefits of handwashing.
Dr Finnikin said: ‘There is no doubt that this whole situation will shine a light on the pressure the NHS is under. I would like to think the public will reappraise their expectations of the NHS and realise the only way it works is if everyone uses the resources responsibly, and that people need to take responsibility for their own health as far as possible. How much this happens only time will tell.’
But Dr Swinyard foresees potential problems: ‘It’s possible that people will recognise that they don’t always have to see us for things. One of the things that worries me is that this might be the final nail in terms of getting any sort of continuity of care. And I would be very sad if that were to happen.’
A nd the profession might also dare to hope that the crisis will bring an appreciation that the huge amount of bureaucracy in general practice is not necessary. The banes of GPs’ lives – CQC inspections, revalidation, QOF tick boxes, online bookings, DESs and LESs – had all been suspended by mid-March.
As GP and Kent LMC medical secretary Dr John Allingham put it: ‘I think some things are being counted, because they can be counted. When all CCG and NHS England staff are working from home or self-isolating, there will be no one to do the counting and they’ll suddenly discover they don’t need to count these things because they don’t actually achieve anything.’
Dr Finnikin said it would not be possible to evaluate the effect of ending inspections and appraisals over this time scale, ‘especially with all the other confounding factors going on’.
But it will allow the BMA to make the case more strongly, once the immediate crisis has passed. As Dr Finnikin put it: ‘At some stage these will be re-introduced and that may be an opportunity to ask (again) whether they are fit for purpose in their current form. It may also be an opportunity for changes to be made without policymakers losing face.’
A vaccine for Covid-19, which could take as long as 18 months, will of course lead to more work for GPs, who will likely have to administer it – another mammoth logistical task.
But, before then, there is a long, harrowing war ahead. There will be many casualties, with GPs no doubt among them. Leicestershire GP and LMC member Dr Grant Ingrams put it starkly: ‘We are going to have to wait and see what’s left, how much of a service have we got left and what we can put back together.’
Reporting by Jaimie Kaffash, Costanza Pearce, Emma Wilkinson and Helen Quinn
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens