Could the profession really turn its back on the NHS?


gpexit graffiti 3×2
This year has not so much given the ‘establishment’ a bloody nose as a compound maxillary fracture.
And, although not on the same scale as the political earthquakes caused by President-elect Trump and Brexit, general practice could be seeing its own revolt.
Many local leaders and grassroots GPs think the writing is on the wall, angry at the failure of the NHS to live up to its promises to help struggling practices and turn around the profession. They have lost faith in the national GP contract and are now taking matters into their own hands.
The most radical solution has been dubbed ‘Plan B’ by GP leaders, and could see GPs ditching their NHS contracts and potentially charging patients for care.
The plans, currently being devised by Northern Ireland GPC and attracting the keen interest of some English LMCs, are at the extreme end of the scale.
But unrest in the profession is growing, with some rebel LMCs cutting funding to the BMA and preparing to conduct their own negotiations to break away from the national GP contract.
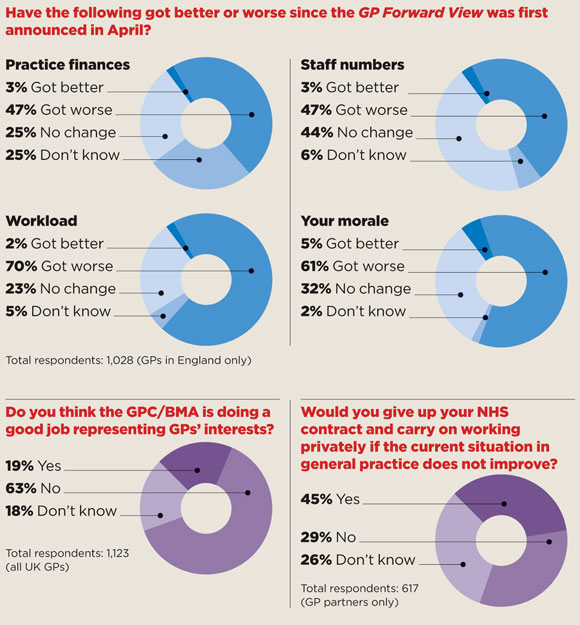
And a Pulse survey of more than 1,000 GPs has revealed a potentially huge groundswell of support for such radical measures. Almost two-thirds of respondents say the GPC is not doing a good job representing their interests.
Meanwhile, 45% of GP partners say they would be prepared to give up their NHS contract and carry on working privately if the situation in general practice does not improve.
At the root of the discontent is the failure of the GP Forward View to make any immediate impact. In fact, most GPs say their position has worsened since the blueprint for the future of the profession was published in March. NHS England promised to ‘turn around’ practices, but 70% of English GPs say workload has worsened since the document was released in April, while 61% say morale has also fallen. Staff numbers have got worse for 47% of GP respondents, and a similar proportion have seen practice finances deteriorate.
This could all be turned around by a blockbuster deal for the 2017/18 contract (due to be published at the time Pulse went to press), but in the absence of such a deal, grassroots GPs and LMCs are demanding extreme solutions.
What GPs are thinking
what gps are thinking box 580x625px
Oxfordshire LMC chair Dr Prit Buttar is preparing a report for Berkshire, Buckinghamshire and Oxfordshire LMCs (BBOLMCs) on a range of radical alternatives for practices in the region, after criticising ‘GPC representation and protection of general practice’.
He adds that his LMC and others are considering ‘everything from one extreme to the other’.
Dr Buttar says the LMC is looking at ‘the economics and the financial reality of what life outside the NHS would look like. How practical is it? How affordable is it? What are the likely consequences for practices and their patients?
‘At one extreme, currently the situation is that you bill patients for HGV medicals and stuff like that, while the state pays for everything else. The other extreme is you walk away from your GMS or PMS contract and set up privately’ – although Dr Buttar says there are ‘lots of shades of grey in between’.
LMCs leaders speaking to Pulse – both on and off the record – report growing disillusionment among their members.
Some of this anger follows the GPC dropping its threat to canvass GPs on industrial action, after May’s LMCs Conference voted in favour of this if NHS England did not meet the demands in the GPC’s Urgent Prescription for General Practice to ease the pressures on GPs.
This document’s demands include setting a cap on the number of patients GPs can deal with in a day, a price list for services that are not covered by the GMS contract and separate contractual arrangements for nursing and residential homes. The GPC dropped the threat of action after legal advice and NHS England’s acceptance of the Urgent Prescription ‘as a good basis for further discussion’.
We are looking at everything… from one extreme to the other
Dr Prit Buttar
But Dr Ian Rummens, medical secretary of Shropshire LMC, which first mooted the idea of undated resignations, says local GPs ‘are unhappy with the way the GPC has failed to respond’ to the call for action. He says the situation has not improved since the LMCs Conference, with ‘most practices one or two resignations away from folding’.
Dr Rummens adds: ‘GPC Northern Ireland has seized the nettle; they know what their GPs think. It is a pity the GPC in London has not given grassroots GPs in the rest of the UK that opportunity.
‘For most GPs, a switch to becoming a private provider is a frightening prospect but the options for remaining sustainable over appear increasingly limited.’
Walsall LMC medical secretary and GPC member Dr Uzma Ahmad can understand the frustrations of grassroots GPs. She says: ‘I do not support Plan B, but I can see where they are coming from. No one wants to take responsibility for what is happening in general practice.’
The fact GPs and LMCs are ready to consider Plan B shows the strength of feeling on the ground, although it is unlikely many GP partners would be willing to risk their livelihoods in this way.
Dr Dean Eggitt, medical secretary of Doncaster LMC, says ‘the GPC has failed to deliver anything in the form of a rescue package’ but describes the idea of handing back contracts to force general practice to become private as ‘ludicrous’.
He adds: ‘South Yorkshire LMCs are developing their own plan B – exploring withdrawing their voluntary levy to the GPC to invest locally,’ and agrees with the suggestion that the money saved could be used to fund local negotiations to replace the national GMS contract.
But for every radical LMC, there is a more cautious one. Other local leaders say they are better off influencing managers by working with them than pursuing fanciful threats that are impossible to push through.
What is Plan B?

Tom Black 300×300
Dr Tom Black – Northern Ireland GPC chair
The Northern Ireland GPC is currently working up a proposal – entitled ‘Plan B’ – involving GPs resigning their NHS contracts and working outside the NHS.
It has already said it will collect undated mass resignations from GPs in protest at underfunding. The move is getting overwhelming support; more than 90% of delegates at recent LMC meetings in Belfast and Armagh backed the proposal.
NI GPC is considering what would happen if those resignations took place, looking at issues such as indemnity, premises, staff, charges, and regulation. It expects this work to take around three to six months.
It is looking at the model in the Republic of Ireland, where there are two types of patients. The first is those with a medical card who are seen in general practice without charge – this is dependent on income and covers around 40% of the population. But those without a card pay a charge of ¤45 to ¤55 for each consultation.
NI GPC chair Dr Tom Black tells Pulse: ‘We already have a situation here in Northern Ireland that one mile as the crow flies from where I am sitting, patients pay to see their GP. The Republic of Ireland model works very well and gets morbidity and mortality statistics that are consistently better than those here.
‘If we have to step outside the NHS then we should make our offer of services direct to patients… Whatever we do we will work very hard to maintain safety and quality of care.’
Oxfordshire LMC has said it is also considering this model, as well as pushing for a change in the law to enable GP practices to charge their own patients for certain non-core services.
Tough job
Cumbria and Lancashire LMCs chief executive Peter Higgins concedes the GPC has ‘an incredibly tough job’. He adds: ‘Half the profession think they’re too soft, the other half that they’re too militant.
‘It’s easy to criticise from the outside without knowing the detail. Negotiating with the battle-hardened NHS England team is never easy and we need to take a hard look at our negotiating levers. A large dose of realism is sometimes needed.’
Northumberland LMC medical secretary Dr Jane Lothian agrees the GPC is doing a ‘good job’ adding: ‘They can’t please everyone – there is no one-size-fits-all solution they can negotiate.’
Meanwhile, Bedfordshire and Hertfordshire LMC chief executive Dr Peter Graves says ‘industrial action of any kind’ would be a mistake. However, the LMC has been extending the services it offers to reflect the ‘new NHS’, including consultancy on issues such as federating and merging. As a result, it has reduced the levy it pays into the BMA.
To be fair to the GPC, it is being more active than ever in encouraging GPs to say no. It recently completed a survey of its membership, asking if practices would consider ‘restricting clinical work to essential services’ or lowering their referral thresholds.
And negotiators hope to announce the new GP contract shortly, which they expect to cover a longer period than one year to provide greater stability, and which could see the QOF scrapped altogether.
The BMA says the frustration of GPs is ‘understandable’, given that politicians of all parties have failed in the past decade to grasp the funding, workforce and workload pressures facing practices.
A spokesperson says: ‘The 2016 LMCs Conference quite rightly expressed anger and asked GPC to ensure the Government accepted the recommendations of our Urgent Prescription, including calls for more funding and an expanded workforce.
‘After pressure from the GPC, this was accepted explicitly by NHS England alongside the commitments in the GP Forward View. The GPC therefore delivered on its mandate, making the call for taking further action not relevant.
‘The BMA is now in direct dialogue with NHS England to ensure delivery of the promises on funding, workforce and workload, and is working in partnership with LMCs to enable local implementation in the quickest possible time frame.’
But speed has never been a virtue of the NHS when it comes to general practice. ‘Plan B’ may look highly ambitious, but in the current febrile environment, nothing can be ruled out.
The view from LMCs
’We’re not particularly impressed with what the GPC is doing to make general practice a more desirable profession to enter’.
Dr Paul Roblin, chief executive, BBOLMCs
‘South Yorkshire LMCs are furious at the GPC’s response to what is happening in general practice’.
Dr Dean Eggitt, medical secretary, Doncaster LMC
‘It’s very easy to criticise from the outside without knowing all the detail and conflicting issues’.
Dr Peter Higgins, chief executive, Lancashire and Cumbria LMCs
‘GPC Northern Ireland has seized the nettle. It is a great pity the GPC in London has not given GPs in the rest of the UK that opportunity’.
Dr Ian Rummens, medical secretary, Shropshire LMC
’I do not support Plan B, but I can see where they are coming from. No one wants to take responsibility for what is happening in general practice’.
Dr Uzma Ahmad, medical secretary, Walsall LMC
’I think the GPC is doing a good job. The GP Forward View will help, but the individual effects are so diluted when they get to GPs’.
Dr Jane Lothian, medical secretary, Northumberland LMC
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens










