Screening by the back door
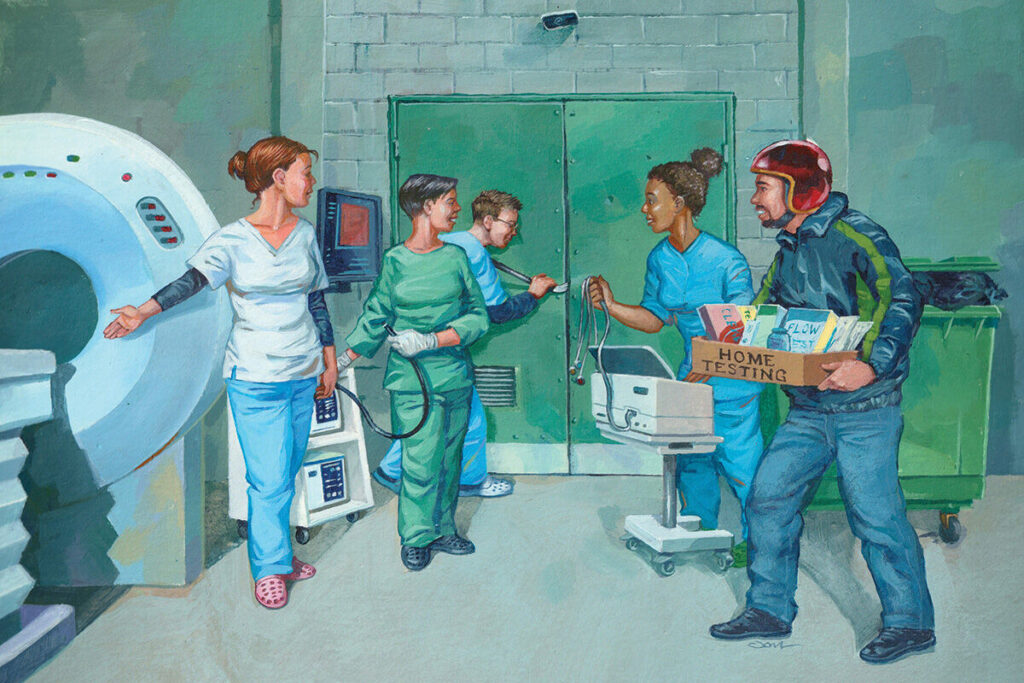
An increasing number of charities and private companies are offering screening outside the approved NHS programmes. Emma Wilkinson examines the effect on GPs
Screening offered on the NHS has to stand up to scrutiny. More than 30 years ago, the independent UK National Screening Committee (NSC) was set up to provide ‘rigorous oversight’ of potential screening programmes, and to consider each on a case-by-case basis and advise ministers. Using Wilson-Junger principles first developed in the 1960s, its main focus is to ensure screening does good, not harm.
Such oversight, however, is hard to communicate to the public. Sad stories about patients diagnosed too late – especially if they are young and photogenic – obscure the nuanced considerations of the harms of false positives and lead-time bias.
As a result, unofficial screening can creep in, contrary to NSC recommendations. Unofficial campaigns by charities or celebrities, health checks offered by private firms and, more recently, home testing kits are among the initiatives of concern.
But not all the pressure comes from outside. The medical profession is bringing in atrial fibrillation (AF) screening, and specialists bang their own particular drum. This has a profound effect on GPs.
Unofficial screening campaigns
This de-facto screening is often driven by charities, sometimes with drug company funding, as well as high-profile individuals ‘recommending’ a test. The most prominent current example is prostate cancer screening with PSA testing. This has always been tricky for GPs to navigate and the NHS has taken an ‘informed choice’ approach.
There are calls for the UK to consider prostate cancer screening and the NSA has said it will explore this further (see box, below). In the meantime, men are being exhorted to get tested. In January, a leading urologist encouraged men to go to their GP to get a PSA test because diagnostic procedures are now more refined and less likely to result in unnecessary intervention. The charity Prostate Cancer UK did a media round proclaiming the benefits of PSA testing now outweigh the harms.
London GP and research fellow at Queen Mary University of London Dr Dipesh Gopal says prostate cancer screening is a difficult issue, but adds: ‘Doing lots of tests to prevent disease doesn’t necessarily improve diagnostics, treatment or outcomes.’
PSA TESTING
In the 1990s, after an NSC review, the Department of Health confirmed that the NHS should not offer prostate cancer screening because of the potential harms. The NHS website states that it has ‘not been proved that the benefits outweigh the risks’.
But there have been calls to reassess. An analysis by Prostate Cancer UK claims the introduction of MRI before biopsy, as well as changes to the way biopsies are done, mean the advantages do now outweigh the disadvantages. And Cambridge University researchers are developing a prostate cancer risk tool they say could help better target screening and diagnostic tests.
The NSC last reviewed the evidence in 2020 and concluded the test was not accurate enough to detect prostate cancer that needs treatment, and could lead to unnecessary procedures. Decisions are reconsidered in three- to four-year cycles and although there has been no formal decision yet, it is understood the NSC will further explore prostate cancer screening, including the possibility of targeting certain groups.
Prostate Cancer UK told Pulse that it believes ‘the balance has now finally tipped in favour of screening – particularly for black men, and men with a family history of prostate cancer, who are at highest risk’.
Meanwhile, the charity Cardiac Risk in the Young (CRY) offers subsidised ECG screening to all young people aged 14 to 35; those found to have abnormal results or symptoms and a relevant family history are referred back into the NHS for further tests. CRY told Pulse it does up to 30,000 screening tests a year.
The NSC does not recommend this screening. Its evidence review showed people can be picked up as positive when they do not have a condition that could cause sudden cardiac death (SCD). The NSC found no research on treatments or interventions to prevent SCD in people flagged by screening, and said it was not known if screening would reduce deaths.
CRY chief executive Dr Steven Cox tells Pulse the charity recognises the impact of a false positive on those being tested and the healthcare system, saying it does not believe cardiac screening should be mandatory. But he insists ‘screening saves lives’.
For many GPs, this simple statement hides more complex issues. One Yorkshire GP – whose name is withheld to protect patient confidentiality – says they were phoned by a parent in a panic after a child was screened at school by CRY. The charity recommended NHS referral for echocardiogram and 24-hour ECG ‘as a minimum’ but the child was fine and the positive test could be explained.
‘I was gobsmacked,’ the GP says. ‘I would have never suggested any of this for this child. In terms of health anxiety, it’s right up there.’
Unofficial screening is also being promoted by the NHS itself. When PCNs were tasked with new service requirements to do opportunistic pulse checks in 2021 for AF screening, the NSC told Pulse it is not currently recommended and it would be appropriate to wait for more evidence.
An analysis last year by Glasgow GP and founder of the RCGP overdiagnosis group Dr Margaret McCartney identified financial conflicts of interest among those promoting AF screening, including charities and academic health science networks.
Private health checks
There are also many companies offering private health screening, either online at home or at a clinic, including investigations such as heart rhythm screening, spirometry, a battery of blood tests and urinalysis.
At Bluecrest Health, people over 40 can have a cancer risk screening check with HPV tests for women (which is not recommended by the NHS outside the cervical screening programme) and PSA for men, as well as H.pylori and FIT testing. Others, including Bupa, restrict PSA to over-50s but offer a mammogram from 40.
An RCGP survey in 2018 found nine in 10 GPs had, in the past year, seen a patient to discuss the results of a private health screening.
As well as being outside NSC recommendations, private tests lead to increased GP workload. Surrey GP Dr Lis Galloway says: ‘Where post-test counselling is offered it is often just advice to “see your GP to discuss further”. We get roughly three to four private reports per week across our team. That’s over 30 hours a year of work that we didn’t create and that private companies profited from.’
Professor Carolyn Chew-Graham, professor of primary care research at Keele University, says: ‘Patients come in and say “I’ve had my private health check, these are the results, can you go through them”. I explain that’s the responsibility of the person who organised the tests and the patient says “I don’t have a follow-up”. I try to be firm but it is difficult when there are abnormalities.’
Sheffield GP Dr Tom Holdsworth says one young patient was referred to him when a private check picked up microscopic haematuria. They had a battery of tests on the NHS, which found nothing.
‘At this point, the patient said “I might not have my health screening next time”, which was what I’d thought all along. There is harm – in the procedures the patient went through and the use of resources. It’s privatised profit but socialised risk because as soon as anything is found, the NHS picks up the pieces.’
At-home testing kits
Since the pandemic there has been a proliferation of companies offering at-home diagnostic kits for a range of conditions and deficiencies.
For online providers, this is usually a kit to take a fingerprick sample at home, which is then processed in a lab, after which the consumer gets a ‘report’ or ‘dashboard’ to view their results.
Last month, the Advertising Standards Agency (ASA) upheld a complaint from Dr McCartney against Numan for its promotion of an at-home blood test offered as ‘free if we don’t find anything’. A spokesperson for Numan told Pulse it has now updated information related to the test on its site.
Last year the Royal College of Obstetricians and Gynaecologists issued a statement advising women not to buy self-test kits for menopause because they are not accurate and only measure FSH instead of looking at the full clinical picture.
The medical community has expressed concern over low-cost at-home tests sold in Tesco via its partnership with UK diagnostic tests provider Newfoundland (see box, below). RCGP chair Professor Kamila Hawthorne warned there is a risk patients will not know how to interpret results or safely act on them, and for something like cancer may not have the appropriate support.
Similarly, the FitBit app provides users with a 30-second single-lead ECG and allows them to get an assessment of sinus rhythm and AF among other features. An Academy of Medical Royal Colleges report in 2019 warned that a ‘feasible outcome’ of the proliferation of such apps is the system being overwhelmed by ‘the worried well’.
The at-home testing kits on sale over the counter
Faecal occult blood (FOB) rapid bowel health (used for bowel cancer screening) FOB tests use a chemical reaction to detect blood in the stool but were replaced by faecal immunochemical testing (FIT) in 2016. But FOB tests are less sensitive and specific than NHS FIT tests. They are also marketed to all ages; FIT tests are currently being extended to 50-74 year olds.
SP-10 male fertility A qualitative test to assess sperm concentration in semen where ‘results less than 15 million cells/ml are an indicator of male infertility’. Infertility investigations are usually not recommended until a couple has tried to conceive for a year. NHS advice is that home test kits have not been widely studied and only check one aspect of fertility so may provide false reassurance or cause needless anxiety.
Vitamin D The rapid self-test measures 25-hydroxyvitamin D in fingerstick whole blood. The Association for Clinical Biochemistry and Laboratory Medicine says vitamin D screening is not recommended in asymptomatic individuals and routine monitoring is usually unnecessary but may be needed where there are persistent symptoms of deficiency or poor compliance with medication.
Ferritin rapid Detects ferritin in fingerstick blood to determine iron deficiency and anaemia. NICE says ferritin tests can be a useful indicator of iron stores in the body, but notes that diagnosis of iron deficiency anaemia requires a detailed history, examination and investigations including a full blood count. It is unclear how accurate the at-home tests are, especially in pregnancy, and ferritin tests require a medical professional to interpret, especially if infection or inflammation is present.
TSH thyroid Detects human thyroid stimulating hormone (TSH) in whole blood to help diagnose an underactive thyroid. NICE says universal screening for hypothyroidism in asymptomatic adults is not recommended although case finding using TFTs is useful in specific clinical situations including pregnancy, a previous history of a thyroid condition, a family history and type 1 diabetes.
FSH menopause (midstream) OTC menopause self-test kits only measure FSH, rather than looking at the wider clinical picture and are not a good method for detecting menopause or perimenopause, the Royal College of Obstetricians and Gynaecologists has said.
No government action
GPs say ‘unofficial’ screening is a growing issue for NHS capacity, patient safety and overmedicalisation. And yet there seems to be little appetite among ministers, the NHS or regulators to push back.
London GP and RCGP overdiagnosis group chair Dr David Spitzer says providers range from ‘well-meaning to cynically preying on people’s health anxieties for financial gain’. Unauthorised programmes may cause ‘significant harm’, he adds.
‘GPs should be encouraged to raise these issues with patients and providers, and only to advise screening in accordance with recommendations of the NSC or other evidence-based programmes.’
The RCGP has issued a position statement of ‘serious concerns’ about screening that is not recommended by the NSC or NICE, and produced a template letter that GPs can use to push back when private providers expect them to follow patients up.3
It states that numerous companies and other organisations are offering screening (without high-quality evidence) that is not recommended by the NSC or NICE. These are carried out in hotels, clinics and supermarkets, as well as online, and have the potential to mislead patients and result in significant cost to the NHS.
The template letter, which GPs can send to a provider explaining the RCGP and BMA position, states: ‘If providers such as yours continue to offer unapproved screening… the RCGP and BMA asks that you ensure that patients are aware of what is, and is not, approved by the UK NSC or equivalent at the point of sale and that you offer follow up of the results that does not put pressure on NHS general practice workload and use limited NHS resource.’
It notes the BMA and RCGP are in discussions with regulators ‘to help to ensure good medical practice is followed by all providers in this area’.
‘Businesses selling non-evidenced or unapproved screening services should not assume NHS GPs will deal with the results,’ says Professor Hawthorne.
The challenge for GPs though is that they have no choice but to discuss abnormal results with patients, leaving themselves open to breach of contract, complaint or even worse (if the results turn out to be significant) if they refuse. North London GP Dr Toni Hazell says: ‘If a patient brings in an unsolicited screening test which is clinically important, I would discuss the likely implications.’
But Dr Hazell says if a patient has simply been ‘taken in’ by a marketing test with no validity then she will explain so they don’t waste more money.
While there appears to be a lack of government action, it seems it is up to GPs to deal with the fallout and try to educate patients themselves. But as long as there are aggressive special-interest groups and private firms seeing a potential for profit without holding the risk themselves, and while there remains an apparent lack of appetite for the NSC or others to take action or apply scientific principles, GPs might be fighting a losing battle.
Related Articles
READERS' COMMENTS [8]
Please note, only GPs are permitted to add comments to articles










I thought such screening tests and investigations were part of the ‘Practice of Medicine’.
The GMC is the regulator for people ‘Practicing Medicine’, and should take appropriate action where a supermarket, hotel, high street store, or online outlet, is found to be ‘practicing Medicine without a licence; and also where a medical charity is offering such testing, but their Medical Director is failing to offer appropriate follow-up.
Most of the tests also require a medical device marketting licence, and would appear to be in breach of this if they are not being administered by a medically qualified person – indeed most of them sytate this explicitly on the package.
Since we are over-run with patients at the moment, there might be little real harm in reporting a few of them to the GMC for regulatory action for ‘practicing medicine without a licence’, and see if GMC decides on some more effective action when it is inundated with complaints from the public as a result.
Great article pulse. Maybe a followup could be to see how many of these companies have MPs as shareholders, or have MPs on the payroll.
How about MRI scanning? This one is the most sinister. Advertised on social media to book yourself for £250 up to £1000 for a VIP service. No referral needed as not “radiation” This will cause chaos, finding brain and renal cysts for starters.
Why stress? Just refer them all to secondary care.
It’s not just screening. The same unscrupulous and profit/public spotlight driven groups are driving the enormous inflation in ADHD and ASC diagnoses, also almost always dumping the patient back on the NHS with no follow-up. I had 1 patient diagnosed in private practice as autistic because they didn’t like the smell of cigarette smoke (clear evidence of sensory processing difficulties apparently) and they found moving house stressful (supposedly demonstrating that they have an abnormally rigid routine)! Sometimes it feels like our job is more about protecting normality than diagnosing abnormality (which the entire world seems to want to do for us)
Slightly off topic but on the subject of unnecessary investigations I continue to be amazed that chiropractors can X-ray patients legally. One that did X-ray a patient of mine was obviously looking for a subluxation (an imaginary diagnosis) and completely missed his metastatic prostate cancer despite serial X-rays to monitor his back pain.
.
Dr No, I once saw a patient who had gone to the alternative practitioner with backpain, been diagnosed with a ‘dislocated vertebra’, had been manipulated to relocate said spinal vertebra dislocation, and still had back pain and leg symptoms (fortunately no perineal sensory loss), and was told to ask me to sign a form for NHS Xray because it was cheaper than a private one. Considering the potential for spinal cord injury when manipulating a spinal vertebral dislocation I just immediately called an ambulance and alerted the local hospital Orthopaedic team to the imminent arrival of a patient negligently treated with manipulation of a spinal vertebral dislocation without prior XRay and Consultant Neurosurgical Opinion (we do not have local Neurosurgery in our DGH).