Smash and grab: how PMS funding is being redistributed


PMS gravestone
Two years ago, Pulse predicted the ‘death of PMS’ in 2016. It hasn’t yet come to pass – but it may not be far off.
Figures obtained by Pulse reveal hundreds of PMS practices have switched to GMS contracts since NHS England began its reviews of the contracts.Two years ago, Pulse predicted the ‘death of PMS’ in 2016. It hasn’t yet come to pass – but it may not be far off.
A quarter (711 practices) have decided to switch to GMS since the reviews began in 2014, in a rapid turnaround of fortunes for a contract that was designed to introduce ‘local flexibility’.
But the additional resources made available to PMS practices were always eyed jealously by their GMS counterparts, and in 2013 area teams were tasked to review £260m of PMS funding – 80% of the extra cash received by PMS practices – that was not clearly linked with extra services above GMS.
Pulse can now reveal how this funding is being redistributed. Responses obtained under the Freedom of Information Act from 116 CCGs show most are throwing it open to all practices – including GMS – in order to fund new schemes to boost access, increase e-referrals or boost elderly care. Others are using it to prop up vulnerable practices.
But the effect on the PMS practices themselves has been drastic. Dr Nick Simpson, a GP principal near Loughborough, moved from PMS to GMS in April, and says his practice will lose about £40,000, but will gain stability.
He adds: ‘You go back to delivering what you might call core [services] such as [treating] diabetes, managing hypertension and dealing with patients who walk in and say they are unwell.’
More specialist services, such as dietitians and possibly vasectomies, will probably have to be cut when a practice reverts to GMS funding, he says.
Other GPs are fighting the cuts. Dr Paul Wilding, a partner at Slaithwaite Surgery in Huddersfield, said his practice’s £277,000 cut amounted to 42% of its budget. He expects to have to cut staff while caring for the same 4,838 patient list. In response, one of his patients has launched a judicial review against NHS England.
Vida Healthcare in Norfolk is losing £550,000 and is having to cut clinical services, but is fighting back with a patient-led campaign, members of which have met with health minister Alistair Burt and told him the CCG did not follow proper procedure before making cuts.
For a number of PMS practices, though, the funding cuts signal the end.
The Practice Group, which covered five PMS practices and 10,000 patients in Brighton and Hove, is having to close, with only one surgery remaining open due to its specialist homeless service.
And in January, senior partners at the Sutherland Lodge Surgery in Chelmsford gave notice of leaving after a £400,000 PMS funding cut. The practice is being taken over by Virgin Care.
Local incentives
But for GMS practices it could be a boon. Most CCGs are using the funding as an incentive to set their own local terms and conditions for all practices, expecting key performance indicators or ‘quality standards’ to be met.
These relate to improving clinical standards and/or improved access, and the CCGs taking this approach include those covering London and Manchester.
A further 26 of the CCGs responding have opted to introduce new locally commissioned services – often related to caring for the elderly or people with long-term conditions, while a small but still significant number said they are using it to create a fund to help vulnerable practices.
Others are spending it on measures outlined in NHS England’s GP Forward View, including broadening the practice workforce and upskilling existing members of staff.
Kent LMC vice-chair and Faversham GP Dr Gaurav Gupta said: ‘It’s essential that CCGs invest the money from the PMS reviews into primary care, so it’s welcome news that some are making plans to do this.’
With funding differentials set to disappear, remaining PMS practices may wonder why they should not plump for the national protection of GMS. It seems as though predictions of the demise of PMS may well have been accurate.
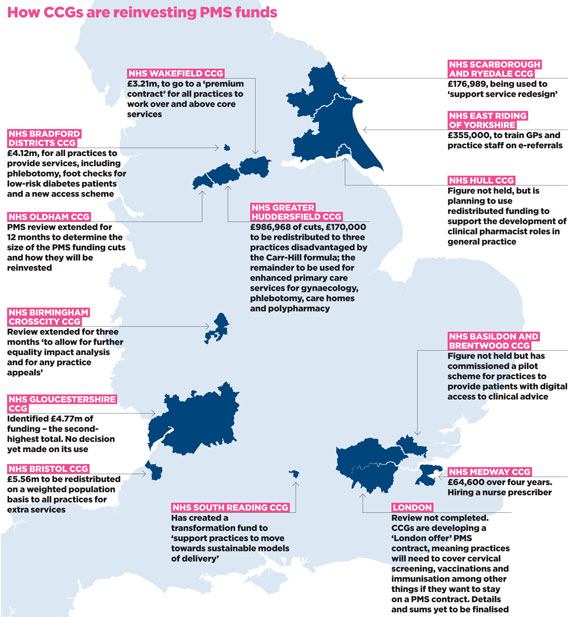
data lowdown map 580x617px
The ‘PMS premium’ funding CCGs are clawing back and how they are pumping it back into GMS
PMS practices are being targeted…
- 3,042 PMS practices in England before the NHS England review
- 711 Switched to GMS contracts by December 2015
- £325m Total premium (funding paid to PMS practices above GMS) identified
- £67m Clearly linked to services over and above GMS
- £258m Not clearly linked to extra services, and therefore being cut
CCGs are deciding how to spend the money they have identified…
- 46 CCGs are redistributing funding via new contractual terms (KPIs, quality standards, quality contracts)
- 26 have commissioned new locally commissioned services, often for elderly or long-term care
- 9 are funding workforce schemes, such as practice pharmacists, nurse prescribing, and staff training
- 7 are spending it on ‘transforming’ general practice or making it more ‘sustainable’
- 5 CCGs completed the review but found no PMS premium that was not linked to services
- 3 CCGs have simply redistributed the cash across all practices
Sources: Pulse Freedom of Information request answered by 116 CCGs in April 2016, supported by CCG board papers in some instances
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens




 Oviva’s fully remote Tier 3 Weight Management programme
Oviva’s fully remote Tier 3 Weight Management programme





