What GPs need to know about the new NICE FIT guidance
Gastroenterologists Dr Michael Colwill and Dr Andy Poullis answer questions about new NICE guidance for colorectal cancer referral
NICE recently published new guidance – DG561 – on the use of the faecal immunochemical test (FIT) to help guide referral for suspected colorectal cancer (CRC). This article answers common questions from GPs.
Why do we need new guidance?
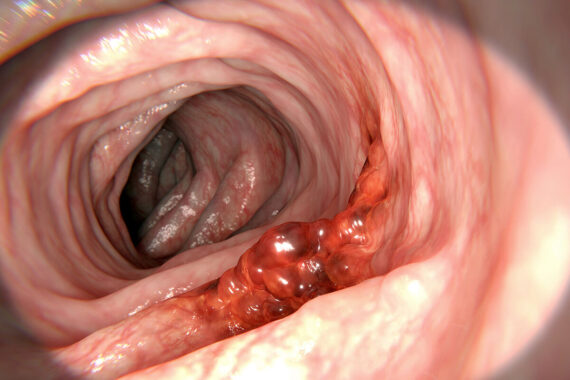
Urgent suspected cancer (USC) referrals for suspected CRC have significantly increased in recent years.2 This has led to strain on endoscopy units, longer waiting lists and a delay in diagnosis and initiation of treatment. NICE has provided new evidence-based guidance designed to streamline referrals by using FIT to identify patients who have a low risk of CRC and therefore do not need an urgent referral.
What is the new guidance?
DG56 states that anyone with the symptoms listed in Table 1 should be referred for urgent FIT using one of two assays: HM-JACKarc or OC-Sensor. If the result is above 10µg haemoglobin/g faeces (µg/g), a patient should be referred under a USC lower gastrointestinal pathway. A FIT should be performed to investigate these symptoms even if the patient has previously had a negative test in the national bowel cancer screening. This does not override a GP’s clinical assessment, so even with a negative FIT, if you have sufficient clinical concern you should still make the referral.
Table 1: When to offer urgent FIT
Offer FIT (HM-JACKarc or OC-Sensor) to guide referral for suspected CRC in adults:
• With an abdominal mass or
• With a change in bowel habit or
• With iron deficiency anaemia or
• Aged 40 and over with unexpected weight loss and abdominal pain or
• Aged under 50 with rectal bleeding and either unexplained abdominal
pain or weight loss or
• Aged 50 and over with any of:
– Rectal bleeding
– Abdominal pain
– Weight loss or
• Aged 60 and over with anaemia in the absence of iron deficiency
Does this supplant the NICE CRC guidance?
Yes, the previous recommendations on when to refer for CRC, DG30, have been replaced by this guidance.
The guidance refers to the use of safety netting if there is a negative FIT but what does this mean in practice?
The guidance advises several strategies including a ‘watch and wait’ process in primary care or a repeat review within a specified time frame agreed with the patient. This repeat review can also be patient initiated if new symptoms develop.
Other options include performing a repeat FIT or referring to secondary care either under an urgent pathway or a USC pathway if there is ongoing clinical concern. What exactly constitutes a clinical concern is left to the clinician’s judgment but is likely to include persistent or worsening symptoms, new symptoms, presence of risk factors such as smoking or a suspicious family history.
How good a test is a FIT?
It is a very good test. A large double-blind, multi-centre study published in 2020 examined 9,822 patients and showed that at a threshold of 10µg/g, FIT had a sensitivity of 90.9% and a negative predictive value of 99.6%.3 A further study from 2020 found five FIT-negative cancers in 477 patients, giving a false negative rate of 1.04%.4 A negative FIT therefore can effectively rule out CRC.
Is there any value in repeating a FIT after a few weeks?
The idea of a dual FIT, where the test is repeated on a separate stool sample within a short time and any positive result requiring USC referral, was considered by the NICE committee as a testing strategy. However, the committee felt that while it increased sensitivity it decreased specificity and would disproportionately affect patients who have difficulty returning a test kit. NICE has advised further research on using dual FIT. While it is not supported yet by evidence, in low-risk individuals with ongoing concern a dual FIT would give further reassurance of the validity of the initial test result.
Should we use FIT in patients under 40 years old?
This is a challenging question where there is little good evidence and NICE has advised that further research is required. The difficulty is that FIT has not been validated in younger patients and so there is no definite certainty about its diagnostic utility in this population. CRC is uncommon in people under the age of 40. However, if you have clinical suspicion, there is no contraindication to performing a FIT. Given that inflammatory bowel disease (IBD) is more common in this age group, a reasonable strategy for patients under the age of 40 presenting with rectal bleeding or chronic diarrhoea is to also test a faecal calprotectin as well as a FIT.
What should we do if patients don’t return a FIT?
This small, but significant and often vulnerable population is identified in the guidance. NICE advises that they should be provided with additional help, information and support in order to return the test.
In reality there will be a number of patients who do not return the test even with additional help, and here clinical judgment and experience are key. NICE also states that further research is required on improving access and return of FITs.
Should we use FIT in the diagnosis of iron-deficiency anaemia?
The new guidance advocates performing a FIT to guide referral for adults with iron-deficiency anaemia or adults over the age of 60 with any anaemia.
Existing NICE guidance on anaemia, which was last revised in April 2023,5 advises USC referral for iron-deficiency anaemia without a FIT in two cohorts of patients: anyone aged over 60 or anyone aged over 50 years who has rectal bleeding; which clearly contradicts DG56.
As the guidance is contradictory, the decision is therefore left to the GP, but a prudent strategy, ideally guided by clinical parameters, is to refer these two cohorts of patients without a FIT. This can be done via a USC pathway as directed by the NICE anaemia guidance. If the referring centre rejects the referral, the GP can reasonably cite ongoing concern as per this guidance.
For patients who do not meet this threshold for bypass, a FIT can be performed. If the test is negative they can be referred to secondary care as per the NICE anaemia guidance.
It should also be noted that a FIT has no utility in non-lower gastrointestinal causes of anaemia and cannot rule out upper or mid-gastrointestinal pathology. Therefore, if there is ongoing clinical concern from a GP a USC referral should be made, as per DG56, and the nature of this concern should be stated in the referral.
What should you do with a negative FIT? The symptoms summarised in Table 1 above provide clear guidance for when to perform a FIT but management after a negative result is a challenge.
A key point to reiterate is that DG56 is guidance only and does not overrule clinical judgment. If there is a clinical concern from the GP then, even with a negative FIT, these patients should be referred urgently.
Safety netting, as discussed above, is also important.
If symptoms persist, GPs can consider urgent referral to gastroenterology or general surgery. GPs should also be aware of bypass symptoms that warrant USC referral without the need for FIT: rectal or anal mass, anal ulceration and specific scenarios involving anaemia, as discussed above.
Dr Michael Colwill is luminal gastroenterology research fellow and Dr Andy Poullis is gastroenterology consultant, both at St George’s University Hospitals NHS Foundation Trust in London
References
- NICE. DG56. Quantitative faecal immunochemical testing to guide colorectal cancer pathway referral in primary care. 2023. Link
- Bradley S. Increases in GP cancer referrals reflect successful health policy, not accidental overmedicalisation. BMJ 2023;381:1349. Link
- D’Souza N et al. Faecal immunochemical test is superior to symptoms in predicting pathology in patients with suspected colorectal cancer symptoms referred on a 2WW pathway: a diagnostic accuracy study. Gut 2021;70:1130-8. Link
- Farrugia A et al. Faecal immunochemical testing (FIT) in symptomatic patients: what are we missing? Frontline Gastroenterology 2020;11:28-33. Link
- NICE. CKS: Anaemia – Iron Deficiency. 2023. Link
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.
Related Articles
READERS' COMMENTS [1]
Please note, only GPs are permitted to add comments to articles










Never take any notice of NICE guidelines———prefer to use my common sense——-which I have in abundance