Key questions: Multiple sclerosis
Key points
- To diagnose MS there must be radiological evidence of brain or spinal cord damage that is disseminated in time (DIT) and disseminated in space (DIS)
- Some 85% of patients with MS have relapsing-remitting disease (RRMS), which causes periods of worsening symptoms followed by full or partial recovery; a much smaller number of patients have primary progressive MS (PPMS) from the outset, where symptoms progress over at least one year, leading to early disabilities
- Consider MS in any patient presenting with features suggestive of neurological symptoms that start and evolve within minutes to days and follow a fixed anatomical pattern
- Common presentations include optic neuritis, transverse myelitis and cerebellar symptoms
- The main benefit of DMTs is fewer and less severe relapses – they reduce relapses by up to 80%
Dr Nassif Mansour is a GP with extended role in neurology in south-west London. Charlotte Casteleyn and Ziad Mansour are fifth-year medical students at University College London
Q: How is the diagnosis of MS made, and what are the main patterns of disease?
A: In MS, an abnormal immune response contributes to focal inflammation in the brain or the CNS and damages myelin. This prevents electrical impulses from transmitting quickly and efficiently, leading to subacute, progressive, localised neurological deficit that plateaus within hours to days and typically improves within a few weeks to months leaving no or mild abnormalities. This process is typically recurrent and can affect any part of the CNS resulting in varied and multiple presentations.
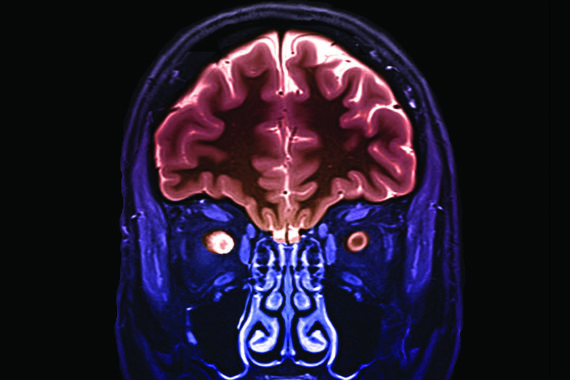
The diagnosis of MS is made through the detection of neurological symptoms, relevant neurological signs on examination, as well as typical MRI changes of the brain and spinal cord, supported by lumbar puncture with oligoclonal bands in the spinal fluid which indicate historical disease activity.
To meet the diagnostic criteria of MS (the McDonald criteria) there must be radiological evidence of brain or spinal cord damage that is disseminated in time (DIT) and disseminated in space (DIS). Sometimes a single event develops, taking years before a relapse happens. In this clinically isolated syndrome (CIS), objective MRI evidence of one lesion will require further evidence of dissemination to eventually lead to the diagnosis of MS. Around 80% of people with CIS develop MS in 20 years.
The most common form of MS is relapsing-remitting disease (RRMS) which characteristically involves periods of worsening symptoms, followed by full or partial recovery – 85% of MS patients have this form. A large percentage of people with RRMS go on to develop secondary progressive disease (SPMS), in which their recovery is halted and symptoms gradually progress. A small proportion of patients have primary progressive MS (PPMS) from the outset. Their symptoms do not relapse but progress over at least one year, leading to early disabilities. Primary progressive MS mostly affects those who develop MS over the age of 40 years while RRMS affects younger people mostly in their 20s or 30s.
Click here to read the full article and download your certificate logging 2 CPD hours towards revalidation
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









