1. Don’t underestimate the problem
Allergic or seasonal rhinitis is estimated to affect up to 400 million people worldwide, with the majority affected before the age of 20.1 The symptoms of sneezing, rhinorrhoea, itch and congestion can affect school and work performance, which can be worsened by suboptimal use of over-the-counter medications causing sedation.
2. Not all antihistamines are the same
Antihistamines remain first-line treatment for mild-to-moderate symptoms and are mainly effective for the symptoms of itching, watery nasal discharge and sneezing. First-generation antihistamines, such as chlorphenamine, are generally more sedating. Sedative effects are reduced in the second-generation antihistamines, such as cetirizine, desloratidine and loratidine, with fexofenadine considered the least sedating.
3. Regular oral dosing is better than as-required use.2
Technique with intranasal steroid (INS) is vital INS is more effective than antihistamines in reducing all symptoms of rhinitis and should be used as add-on therapy in moderate-to-severe symptoms. Patients will generally start to see an improvement in symptoms after two to three days’ use, although it may take up to two weeks to have full clinical effect.
A common reason for treatment failure is that the technique of administration has not been clearly demonstrated to the patient. Remember the ‘head down’ approach with the nozzle of the spray pointing upwards – one or two sprays into the nasal cavity with a gentle sniff.
All INSs have a similar clinical benefit. However, systemic bioavailability is variable – long-term growth data in children are reassuring for fluticasone, mometasone and budesonide, but growth suppression has been identified with beclometasone.3
4. It is important to start treatment at the right time
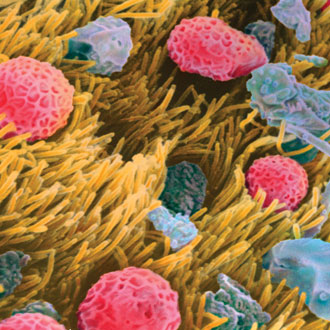
Although the most common indoor allergen causing allergic rhinitis is the house dustmite (generally perennial symptoms), most people with seasonal symptoms are reacting to pollens. The early tree pollen season (for instance, birch pollen) tends to start in late March through to mid-May, grass pollens (such as timothy grass) between May and July, and weed pollens (ragweed) from June to September. Fungal spores such as aspergillus can cause autumnal symptoms.
Benefit has been shown with INS when starting treatment two weeks before a known allergen season.4
5. Testing can be helpful to both clinician and patient
Access to allergy testing in primary care has always been variable. Some areas have good coverage, with allergy clinics for all ages. Generally, skin-prick testing has only been available in secondary care but there is often good availability of specific-IgE blood testing to GPs across the UK.
Positive responses to skin-prick testing or high levels of specific-IgE in the blood confirm sensitisation to the allergen rather than confirming allergy (so patients may be sensitised to an allergen but show no clinical allergic response to it).
It is important that such tests be done cautiously and in the context of a clinical history of allergic response.
Such testing can help to tell patients when to consider starting treatment and whether a pet at home may be a trigger, and to help exclude an allergic cause to the symptoms.
6. Nasal douching is cheap and effective
Saline nasal-douching kits are easily and cheaply available online or at larger pharmacies. This is a safe and effective treatment for symptomatic relief and one that is used more commonly across Europe than in the UK.
A Cochrane review in 2007 concluded that, although it was not as effective as an INS, saline irrigation was well-tolerated by both adults and children, and beneficial for symptoms of nasal and sinus congestion, even as the sole method of treatment.5
7. There is a significant link between rhinitis and asthma
A number of studies have shown important links between the two:
• It has been shown that asthma patients who receive appropriate treatment for rhinitis have a significantly lower risk of A&E attendance and hospitalisation for their asthma.6
• Rhinitis is an independent risk factor for the development of asthma.7
• Up to 80% of patients with asthma have symptoms of rhinitis.1
• Consider adding questions about symptoms/treatment for rhinitis to asthma review templates.
8. Anti-leukotrienes (LTRA) can have a role in some patients
The British Society for Allergy and Clinical Immunology’s Guidelines for the management of allergic and non-allergic rhinitis2 suggest add-on therapy with an LTRA (such as montelukast) in patients with seasonal allergic rhinitis and concomitant asthma. LTRAs are thought to be as effective as antihistamines in some patients, though less effective than INS.
9. Be aware of pollen food syndrome
Also known as oral allergy syndrome, some patients with seasonal rhinitis can experience allergic symptoms, usually oral in nature, to a wide variety of fruit and vegetables. Although they are unlikely ever to have a severe allergic reaction, the symptoms can be unpleasant and confusing.
The most common allergen responsible is birch pollen (Bet v1), which cross-reacts with a large number of different foods (such as peach, kiwi, apple, almond, hazelnut, soya). Referral to an appropriate allergy service with dietetic support can allow the patient to be aware of what foods will affect them.
10. Consider referral for patients with suspected occupational rhinitis/asthma
Referral to specialist services should be considered in all patients with suspected occupational rhinitis/asthma, and all children with the combination of suspected food allergy, rhinitis and asthma. Access to allergen-specific immunotherapy is improving across the UK and there is increasing use of hyposensitising agents, such as Grazax (grass pollen immunotherapy), which is licensed from five years of age. Referral to an age-appropriate allergy service can help patients access these treatments.
Dr Matt Doyle is a GP in Cambridgeshire and chair of the British Society for Allergy and Clinical Immunology primary care group