The case
A 34-year-old taxi driver developed a sudden, severe pain in his anus while driving his cab. The pain made him feel light headed and he needed to pull the cab over to the side of the road. After a minute or two, the pain gradually subsided and then disappeared completely. He was able to resume driving and did not have any other problems for the rest of the day. A few months later he developed a similar anal pain after opening his bowels and he needed to lie down for several minutes until the pain disappeared.
Definition
Proctalgia fugax is a spasm-like pain in the anal canal that occurs infrequently and typically lasts for only a few minutes. The aetiology is poorly understood but it may occur secondary to spasm in the muscles of the anal canal or pelvic floor. The diagnosis is made from the characteristic clinical history and by excluding other causes of anal pain. As the attacks are short-lived, treatment is usually unnecessary.
Proctalgia fugax can be defined as an intermittent and self-limiting pain in the anorectal region in the absence of organic pathology. It was first described by Myrtle in the British Medical Journal in 18831, whereas Thaysen, a Danish physician, was the first to use the term proctalgia fugax (fugax from the Latin for fleeting).2
Diagnostic criteria and differential diagnosis
Proctalgia fugax is regarded as part of the functional bowel disorder spectrum, and diagnostic criteria are listed in the table below. By definition it causes pain that lasts for 30 minutes or less. Functional anorectal pain lasting more than 30 minutes is classified as levator ani syndrome when there is associated tenderness on palpation of the pelvic floor muscles, or unspecified functional anorectal pain when there is no associated tenderness.
Diagnostic criteria for proctalgia fugax
- Recurrent episodes of pain localized to the anorectum
- Episodes last from seconds to minutes, with a maximum duration of 30 minutes
- There is no anorectal pain between episodes
- Exclusion of other causes of anorectal pain
Prevalence
Most patients do not seek medical attention so the true prevalence may be unknown, but a population study found that proctalgia fugax has a prevalence of 8%, is equally common in men and women, and occurs more often in patients younger than 45 years of age.3 Studies in patients referred for treatment, however, typically show prevalence in females and a slightly older age of presentation. Although it has been reported in children, it is thought to be rare before puberty.
Clinical features
Patients often describe a characteristic history of a sudden, severe pain in the anorectal area that lasts from a few seconds to several minutes and then disappears completely. It is usually described as a sharp, stabbing, or spasm-like pain. Attacks are infrequent, typically fewer than five times per year, although some patients can have pain every day. Often patients have to stop what they are doing and wait for the attack to subside. Many patients describe symptoms occurring at night. The pain tends to occur spontaneously without a trigger, but some patients describe aggravating factors such as sitting down, defaecation, or psychological stress.4 Similarly, relieving factors are mostly absent but lying down, relaxation, heat application, and digital pressure to the anal region have been reported. One study reported that in 7% of patients the pain radiated to other areas such as the buttock or pelvis, and in 19% there was an associated symptom such as sweating or feeling faint.5 A proportion of patients describe passing out due to the severity of their pain.4
It has been suggested that there is a correlation with an anxious personality type, as well as a possible association with other functional gastrointestinal disorders, such as irritable bowel syndrome. An estimated 80% of patients with the condition do not seek medical attention as their symptoms are not too troublesome3, and the natural history of the condition is probably unknown but some patients continue to have symptoms for many years.
Pathophysiology
Although the true cause has not been fully determined, many studies suggest it is due to an abnormal smooth muscle contraction in the anal sphincter or pelvic floor. The sensation of pain has been shown to correlate with high amplitude, high frequency myoelectrical activity of the anal sphincter. Anal resting pressure is mainly derived from internal anal sphincter tone, and pain levels have been shown to reduce in line with resting pressures after biofeedback aimed at relaxing the anal sphincter. It is plausible, therefore, that proctalgia fugax is due to a paroxysmal smooth muscle hyperactivity and hypertonia.
Slow wave activity within smooth muscle is increased by sympathetic activity, and this may explain the correlation with stress. A third of patients seeking medical attention for their symptoms have been shown to have a family history of proctalgia fugax,4 and a rare autosomal dominant familial form has been described with constipation, in which family members have increased anal pressures and thickened internal anal sphincters.
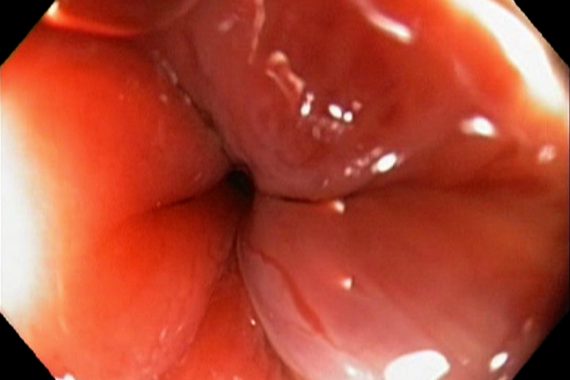
How can GPs diagnose with certainty
The diagnosis is made from the characteristic clinical history together with exclusion of other causes of anal pain. Pathologies such as anal fissure or fistula, haemorrhoids or perianal haematomas, and anal cancer can all be associated with pain, but symptoms are more frequent, longer-lasting and associated with abnormalities on examination. The pain of an anal fissure is almost always initiated by defaecation but can last for many hours afterwards. A fissure can be difficult to diagnose on external anal inspection but is usually visible after gentle stretching and eversion of the anal margin.
When to refer
Most patients are happy to accept the diagnosis once other, more significant pathology, is excluded, especially if attacks are infrequent. If there is doubt over the diagnosis or if symptoms are frequent or severe enough to interfere with a patient’s quality of life and conservative measures have not helped, a referral to secondary care for further investigation and management would be appropriate.
Mr Gary Atkin is a consultant colorectal surgeon at the Lister Hospital, East and North Herts NHS Trust
References
1. Myrtle AS. Some common afflictions of the anus often neglected by medical men and patients. BMJ 1883;1: 1061 – 2.
2. Thaysen TE. Proctalgia fugax. Lancet 1935;2:243 – 6.
3. Drossman DA, Li Z, Andruzzi E, Temple RD et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38(9):1569-80.
4. Atkin GK, Suliman A, Vaizey CJ. Patient characteristics and treatment outcome in functional anorectal pain. Dis Colon Rectum 2011;54(7):870-5.
5. de Parades V, Etienney I, Bauer P et al. Proctalgia fugax: demographic and clinical characteristics. What every doctor should know from a prospective study of 54 patients. Dis Colon Rectum 2007;50(6):893-8.
6. Eckardt VF1, Dodt O, Kanzler G, Bernhard G. Treatment of proctalgia fugax with salbutamol inhalation. Am J Gastroenterol. 1996;91(4):686-9.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens




 Oviva’s fully remote Tier 3 Weight Management programme
Oviva’s fully remote Tier 3 Weight Management programme






