Smashing the ten-minute tyranny


smashed clock face 3×2
The idea of 15-minute appointments has been the holy grail for GPs for years.
But from being a seemingly impossible ideal, it has become the focus of the GPC’s strategy for making general practice sustainable again.
It proposes the ‘radical solution’ of a cap on the number of patients a GP can see in a day at 25. To make this happen, it has suggested health managers commission ‘overflow hubs’, where GPs can send patients with urgent problems for same-day appointments when their own practice is full.
Under the plans, the role of the standard GP practice will centre on dealing with patients’ long-term conditions. Same-day urgent – but not chronic – health conditions, such as earaches, infections and minor injuries, will be left to the multidisciplinary teams in the hubs when the practice reaches the 25-patient limit.
The GPC stresses that ‘hubs’ are no panacea, and that there are other ways to end the 10-minute appointment treadmill.
But it looks as though the hub idea is taking hold, with at least five areas across England already commissioning such hubs. Even more importantly, NHS England has told Pulse it is keen to roll out this model across the country.
GP leaders say this will make a ‘fundamental’ difference to the working lives of GPs.
Continuity at risk
But not everyone is so enthusiastic. Critics say the hubs will not deliver longer appointments as the depth of the crisis in the profession means practices do not have time to establish them and they will have the unintended effect of diminishing continuity of care.
Most alarmingly, in areas where such hubs have been set up, they have become full themselves and sent their overflow patients back to GPs and it is unclear how they will be funded.
The plan supports NHS England’s GP Forward View, which sees large groups of practices taking forward an expanded role for general practice, but those outside such structures could be left behind and perhaps see their own funding reduced as a consequence.
The GPC says collaborative working is the best way to cut workload.
GPC chair Dr Chaand Nagpaul says: ‘We do need some radical solutions to limit workloads.
‘Given that NHS England has earmarked significant funds for transformation, we believe this would be an appropriate call upon that resource. It links in with the GP Forward View’s own comments on resourcing locality hubs.’
For GP leaders, there is a lot riding on successful implementation of 15-minute appointment slots. In August it shelved the idea of balloting GPs on industrial action after it claimed it won concessions from NHS England on aspects of its own Urgent Prescription for General Practice. A cap on appointments and the introduction of 15-minute slots are the flagship policies of that document.
And so far, so good for the GPC, which has been heavily promoting the idea over the past month, with some success. It has been across the mainstream media, including the front page of the Guardian and TV news.
The GPC elaborated on its ideas in its Safe working in general practice plan, launched in August. The document says: ‘The immediate introduction of 15-minute appointments would allow improved decision making and case management, and should reduce the administrative burden outside clinic times by facilitating more activity within the appointment.
‘As patients increasingly present with more complex conditions, longer consultation times are necessary to ensure safe and high-quality patient care.’
In principle, there is nothing currently stopping GPs from offering 15-minute appointments, but in practice this can only be achieved by limiting workload.
A review in last January’s BJGP by GPC member and Shropshire GP Dr Mary McCarthy of countries where ‘general practice workload is reasonable’ found that the ‘most important factor is the number of patient consultations per GP per day’. Dr McCarthy concluded that the answer is to ‘restrict patients contacts to fewer than 25 a day’.
Overflow hubs could be the vehicle to enable the setting of ‘limits to working days’, the GPC concludes. The hubs will be staffed by other healthcare professionals, such as advanced nurse practitioners and pharmacists, to ‘minimise the number of GPs needed’.
Crucially, it says the funding should come from the additional £2.4bn a year earmarked for general practice by 2020 in the GP Forward View.
And this is no vague policy idea – already at least five areas are using money from various Government and NHS England initiatives to establish overflow hubs. And many of the new ‘sustainability and transformation plans’ – the secretive plans on the future of health services in the 44 regions in England – set out proposals to introduce such hubs.
Members of the GPC are promoting the idea in their local areas. Dr Brian Balmer, GPC lead on this issue, says: ‘It will be the first time we integrate primary care, while preserving existing practices and allowing them to control their workload.’ He is in negotiations with his local CCG ‘to commission a hub to pick up the slack’, in the hope it can get up and running in the next six months.
This allows practices to control their workload
Dr Brian Balmer
In Stoke-on-Trent, GPC member Dr Chandra Kanneganti has helped launch an overflow hub this month. ‘It will not immediately mean we can offer 15-minute appointments, but that is what we are working towards,’ he says.
NHS England is open to the idea, with a spokesperson telling Pulse: ‘ We are exploring the idea of overflow hubs with the GPC as part of ongoing discussions aimed at further supporting practices and improving services for patients.’
Head of general practice development Dr Robert Varnam tells Pulse such ideas are ‘definitely under discussion’.
‘We were talking about this in my practice 10 years ago, but one of the things that has happened through the Access Fund [announced by former Prime Minister David Cameron to boost seven-day access] in the past couple of years is that some practices have actually done it, and they’ve shown it is feasible.’
Dr Varnam says existing schemes have had ‘teething issues’, but adds: ‘By and large it looks like it does really work.’
However, he says it will be up to local practices to set up these hubs: ‘Practices themselves have to agree they are going to do that. No one could force them to do it.’
But critics have pinpointed this as the fundamental problem.
Dr Shaba Nabi, a GP in Bristol and a board director of Avon LMC, says: ‘It’s a joke, it‘s a complete joke. There aren’t enough people to staff it.
‘What you are doing in fact is reducing continuity of care, a crucial element of urgent care. You can’t separate long-term care from urgent care.’
Dr Nabi says staffing hubs with non-GPs will be inadequate: ‘It would be lovely if you could guarantee all patients presenting are clinically appropriate for those other people. But you could be sending patients with life-threatening issues or mental health issues, and they are completely unequipped for that.’
And in practice, such issues are already causing problems. Dr Dean Eggitt, medical secretary of Doncaster LMC, points out another fundamental issue: ‘We have a local overflow hub and it is already at capacity. As such, patients are being sent back to GPs.’
No panacea
Indeed, while Family Doctor Association chair Dr Peter Swinyard concedes that his local hub has its uses, he says it is only a sticking plaster. Most importantly, he warns, it could eventually reduce other practices’ funding. And GPs have been here before, with large Darzi walk-in centres sucking up cash when they were introduced in every area from 2007.
He says: ‘Inevitably funding has been diverted to these centres from that available to the CCG for general practice. And I do wonder if it wouldn’t have been better to put the money into general practice and allow us to find solutions, and employ people to treat patients.’
Even if funding does come from the cash pledged by NHS England, it will be administered by CCGs – with many stating they will only commit funding to large practices and federations. Even Dr McCarthy acknowledges ‘overflow hubs won’t be the answer everywhere’. She says: ‘It’s fine for a city, not for Shropshire where I work and practices are miles apart.’
The GPC does acknowledge problems with the idea. Dr Nagpaul concedes hubs are no ‘panacea’ and says ‘we are not being prescriptive and saying this is what has to happen’. However, he says the GPC is calling for new money to support the proposal: ‘It is an important option to limit workload to have longer consultation times and for excess work to be absorbed outside the practice.’
Hard-pressed GPs around the country will hope he is correct.
How the overflow hubs will work
The GPC has explained how the hubs could work in local areas. It has also highlighted five existing schemes to date, funded via the Prime Minister’s GP Access Fund and NHS England’s vanguard programme
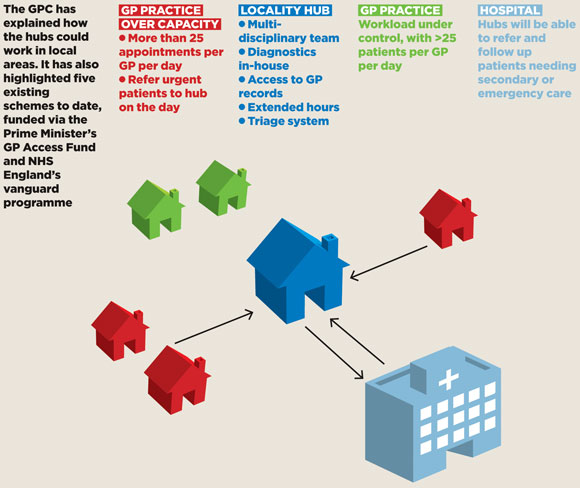
gp hub diagram 580x488px
Where are they working?
1 Lambeth, south London
Four hubs, run by the Lambeth GP Federations, offer GP and nurse appointments, face to face and via telephone, 8am-8pm on weekdays and 10am-6pm on weekends and bank holidays. Patients are referred for appointments if there are none within 48 hours at their registered practice or if they cannot attend during regular hours. The project received £3.5m set-up costs from the GP Access Fund and £1.5m from NHS Lambeth CCG
2 Southwark, south London
Two GP federations operate two hubs covering 22 GP practices each, offering same-day urgent care appointments 8am-8pm seven days a week. Patients with complex conditions are encouraged to attend their registered practice. The out-of-hours provider can also refer patients to the hub. Funded by around £1m from the GP Access Fund and £2.1m recurrent funding from NHS Southwark CCG
3 Gosport, Hampshire
A multispecialty community provider (MCP) vanguard is piloting a hub covering four GP practices with 39,000 patients, offering appointments with GPs, advanced nurse practitioners and emergency care practitioners 8am-7pm Monday to Friday.
4 New Forest, Hampshire
Seven GP practices have set up a hub covering 70,000 patients. It offers GP and nurse appointments, both urgent and bookable, 8am-8pm seven days a week. Staff include GPs who are recently qualified or partially retired. Funded by £800,000 from the GP Access Fund
5 Oxfordshire
The PML GP Federation is piloting six hubs offering same-day GP and advanced nurse practitioner urgent appointments. It is intended to be an overflow facility to free up practices to offer routine appointments and longer consultations for complex conditions. It covers 35 GP practices and 350,000 patients. It is funded from the region’s GP Access Fund allocation of £4.9m
Source: Safe working in general practice. GPC, August 2016
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












