ICB considering ‘111 First’-style GP access model

Exclusive An ICB is working on plans to overhaul its GP model, which would see patients triaged by 111 call handlers and seen in a ‘neighbourhood hub’.
GP leaders have raised severe concerns about the radical plans, which Pulse understands Hampshire and Isle of Wight ICB is working on for an April 2025 introduction.
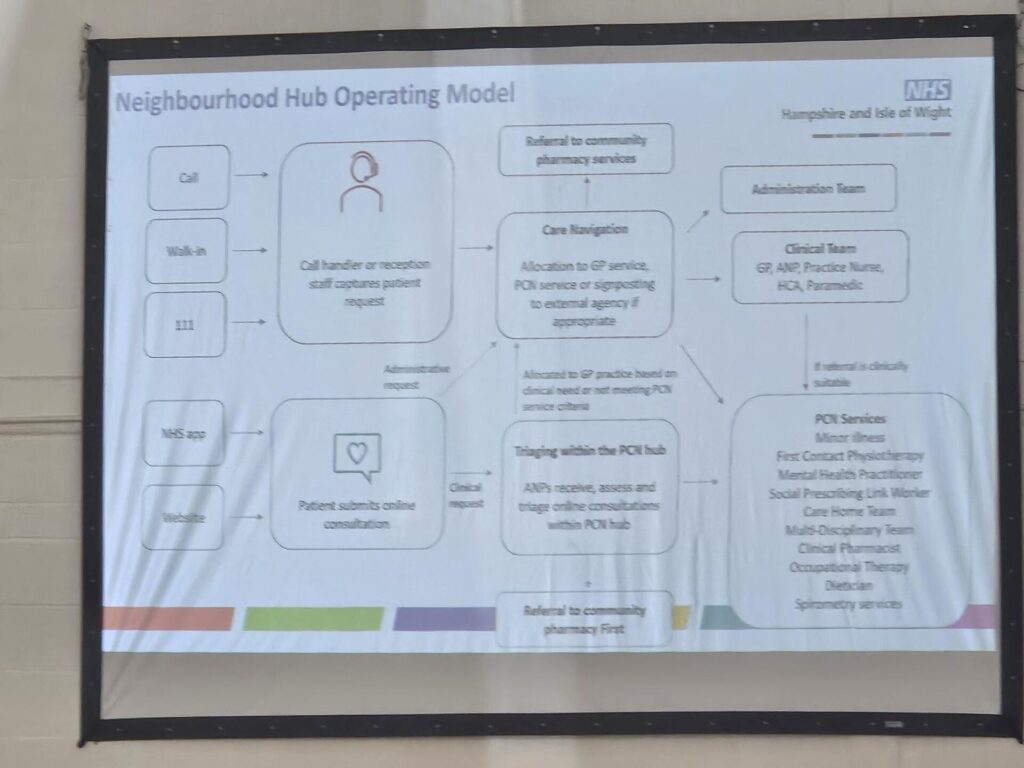
Similar to plans which have been put on hold in North West London, the ICB is looking at a Fuller stocktake-influenced ‘neighbourhood hub operating model’ from next year.
But in a set-up reminiscent of the ‘111 First’ model for A&E triage, which has been piloted by NHS England, this would include access through NHS 111, where a call handler would capture the patient request and ‘allocate to GP service, PCN service or signposting’.
Patients would also be able submit online consultation forms and be triaged within the ‘PCN hub’ to then receive care from ‘PCN services’, according to a chart created by the ICB and seen by Pulse.
Pulse was told that the plans ‘will be incentivised both through national and local contract leverage’ but the ICB refused to respond when asked what this means in practice.
A spokesperson told Pulse the ICB is ‘considering’ the hubs but plans ‘are not yet finalised’ and there is ‘no agreed date’ for implementation at this stage.
A GP who asked to remain anonymous told Pulse the plans by Hampshire and Isle of Wight ICB caused ‘a lot of sleepless nights’ as well as ‘anxiety and concern’ about what this means for practices.
They said: ‘The question is: where do GPs sit in this? They would sit primarily in the care navigation component and they call that a “GP service” within the PCN. There is no mention there of GP practices.
‘There is anxiety and concern about what this means. We are not just looking at the loss of local GP surgeries, this changes access, and care is no longer delivered in the local community.
‘And it also changes the professional makeup of being a GP – it seems like the role that they are intending to implement involves less patient contact and more to do with supervising the additional roles.’
They added that practices are ‘desperately thinking about their alternative options’, including outside the NHS.
GPs also expressed concerns that the plans were looking at replacing practices’ GMS contracts with ‘PCN level contracts’, but the ICB refuted this and told Pulse it ‘currently has no plans to replace any current GMS contracts’.
Dr Kieran Gilmartin, who has recently stepped down as a clinical director of Fareham and Portchester PCN, told Pulse that there are concerns GPs ‘are being forced’ into the plans.
He said: ‘We recently had a meeting with the ICB – it’s the fourth one we had in the past 12 months and they brought up this model they call “neighbourhood hub operating model”.
‘All of what they put on there we already do, and we have PCN services – we do have social prescribers, home visiting team, clinical pharmacists – we have a lot of other services that people can either directly book into or are triaged into.
‘The concern is that we are being forced into something that we know isn’t the best and isn’t the right thing for patients.
‘We have proven that continuity is important for certain things and actually knowing your patients means you get through them quicker, and you actually provide them with a better service if you know who they are.
‘There’s so many concerns around it – and that we are not really being spoken to like adults. The concern is that general practice won’t be here in any format similar to what it currently is in the next 12 to 24 months.’
The ICB’s director of primary care James Roach said: ‘The introduction of neighbourhood hubs across Hampshire and the Isle of Wight is an option that we are currently considering, however plans are not yet finalised and there is no agreed date for implementation at this stage.
‘We are looking at developments across the country and are seeing how the neighbourhood hub models are working in other areas.
‘Any changes we make to our primary care model will have local people and local needs at the centre of any decision making.
‘Access to local care remains our priority and we continue to engage with our PCNs and practices on potential service developments.
‘We currently have no plans to replace any current GMS contracts in Hampshire and the Isle of Wight, but we recognise the challenges that the most recent contract iteration presents to our practices.
‘We are working collaboratively with our practices and PCNs to ensure we can support them effectively and we are looking at how we can ensure that there is further investment into primary care.’
It comes after North West London ICB was forced to shelve similar plans for same-day access hubs, aimed to ‘deliver a single point of triage for same-day, low complexity’ demand for all 2.1 million residents within the integrated care system, leaving GP practices with only longer-term, ‘complex’ care.
It is however still planning to overhaul its primary care model by April 2025 and it has indicated it will not consult on plans as same-day hubs are a ‘national imperative’.
When asked about NWL last month, NHSE’s primary care director Dr Amanda Doyle said she wants to ‘step back’ and let local systems get on with proposals to overhaul same-day access.
Pulse has reported on other areas implementing similar models, including in Cornwall where retired GPs will staff hubs to ease on-the-day demand, and Oxfordshire where ‘non-complex’ patients will be dealt with at same-day hubs.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [16]
Please note, only GPs are permitted to add comments to articles













I’m not sure why anybody is surprised by this direction of travel. Everything has been pointing to this but us and our negotiators have buried our heads in the sand. Even when we gave small amounts of appointment access over to 111 a few years ago everyone said it didn’t really matter but it was just the start of all this.
The GP model we know will absolutely be gone very soon and the profession needs to decide whether they want to work in this or seek an alternative model.
For anyone close to retirement it doesn’t matter but for our younger GPs it will be a completely different job and PCN CDs and our representatives who are close to retirement need to pause and stop enabling this until our younger colleagues have had a voice.
Unless you have skin in the game for the next 10 years or more you need to let the younger generation decide.
Seems to me we are basically in the midst of scrapping general practice and replacing it with a half arsed hospital inspired outpatient/a&e minors model staffed by paramedics and PAs coordinated by 111 ..its not been openly discussed and agreed with the country at large its just happening. Don’t like it? Tough shit
Andrew, I agree with the points you are making regarding the direction of travel. Only thing, there is no enabling this from our side. No one is asking the profession, all is happening in the good usual nhs style top down way.
James Roach says taking the views of local people in to account. Does his ICB actually have any ‘patients’ on it?. Ours does not nor any PPG reps and in fact very little connection with primary care. Nowhere in this discussion are the views and wishes for patients. One assumes there are dictats coming from NHS England with their very own ‘agenda’. Can those working GP who advise politicians and NHSE be named and interviewed as to the real final solutions they see GP land in 5 years I am now more interested as being receiver rather than a provider care
Well I work in GP surgeries, 111 out of hours and as GP in a large A&E (the latter to deal with the deluge of crap 111 signposts to ED) and this will have a massive impact on hospitals; everything will get sent in and primary and community care will fall apart. 111/out of hours provides awful crappy care to generally the younger more straight forward patients. This is going to be a big disaster. My A&E are trying to get an urgent care centre run by GPs up and running in the hospital to deal with the diversion of primary care into A&E that is already occurring. A&E is at breaking point. This will finish off the NHS and secondary care. These managers are morons.
‘Unless you have skin in the game for the next 10 years or more you need to let the younger generation decide.’ (Tend to agree but so many of the younger people seem to be heading for sunnier climes).
111 are very poor.Usual NHS promote failure, where most of the top managers come from.
Every GP knows and feels viscerally that GP tradition has combined both science and art in their daily work, with balletic or melodic grace. The same narrow minded thinking by DHSC management boffs would no doubt parcel out Swan Lake, or Mozart’s 41st, and then wonder why the result they got was an unforgivable mess.
Has anyone evaluated the effect of “111 First” on A&E before extending it to mainstream generell practice? It doesn’t seem to have been conspicuously successful.
111 need to be scraped. I tried it twice for myself and did not even reached to talk to any one.
All very sad that a high quality service has been reduced to this . Not only have GPs not been asked but neither have the general populous . Gps have lost a lot of the diversity of their practice and with it job satisfaction and the patients have lost the ability to self care and decide for themselves when they need to access healthcare . 111 triage vast numbers of patients inappropriately so providing false education of when to access primay care or emergency care .By trying to reduce primary care patients in ED perfect pathways have been put in place to completely bypass primary care pathways ie 111 callback waits , appointment waits etc and patients now turn up in ED hoping to be diverted to the co-located GP service . It s not a nil sum game as it creates big triage waits and puts seriously sick patients at high risk of harm. Patients need to be re-ebabled to make their own decisions we can’t afford a system that Totally Triages every individuals cough or pain .
I am close enough to retirement to hang on until I get out but the thought of being looked after in older age by a system reliant on remote triage, email consults ,noctors and zero continuity terrifies me and so I suspect I will do exactly what all the current changes are designed to do: pay for a private GP. via a private medical insurance policy
…….and the headline today is how satisfaction in the NHS has dropped from 70% to 24% in 13 years. QED…
Our practice has triaged patients for the past decade.
We believe that triaging should take place via the most experience clinicians, not the least experienced. That ensures the patient is most likely to see someone from a service that is appropriate – physio self referral, community pharmacy, physician associate, practice nurse, ST1 Dr, ST3 Dr, nurse practitioner, dentist, named GP who is handling that patient etc, clinician with particular competencies e.g. family planning etc. We look for patients with non resolving issues that need continuity or an experience GP to review them. We are able to identify and prioritise end of life and vulnerable patients. Where patients contact reception to complete the triage info the local knowledge they have is invaluable in identifying patients we know are complex or vulnerable also. Our ARSS staff work in the practice and are part of the team, rather than remotely in another service, and come to our daily clinical meetings that include reception and admin supervisors.
111 triage is traditionally over cautious and contributes massively to ambulance call outs. 111 are entirely unsuited to being the front door for the complex problem that is matching changing patient health needs in an appropriate time scale to the varying capacity of the practice to meet this, with staff whose competencies at a given time are far more granularly defined than just ‘GP’ or ‘pharmacist’ etc.
Change happens, people complain, people get over it, others don’t, others make lemonade. GPs however only think about pension pots and profit. Let’s not just blame the Tories.
There is a real problem on the commissioning side that constantly feels it has to duplicate services to solve a problem rather than invest in the systems that are there already. This generates supply induce demand which becomes a spiral into biomedicalising everything thing and the unaffordable costs that go with this. One in five adults in england and one in four adults in Scotland are on antidepressants with little evidence of benefit in mild to moderate depression. We are now doing the same with pharmacy “second”. Most is mild self limiting illness.
111 first has been a massive backwards step for urgent care triage. We get so many inappropriate patients from them in our UTC, and patients often know it.
Basically primary care / urgent care is in a mess, and nobody knows what to do.
Not helped by the fact that this ICB seems to be in a total mess – they have made so many staff redundant, and often the remaining staff do not seem to know what is going on.