2021 Review: The mid-pandemic workload crisis
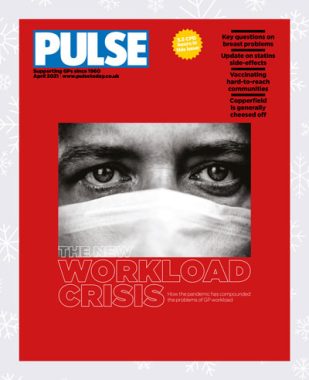
Workload crises are not a new situation for GPs, but this year’s crisis was different. Allie Anderson continues our review of the year
There have been GP workload crises before. In 2019, GPs who took Pulse’s seminal workload survey reported they were working unsafe hours.
Two years on, everything has changed – yet nothing has. Deep into the Covid-19 pandemic, the world is unrecognisable, but general practice is facing similar unrelenting challenges. One workload crisis has made way for another.
In our 2021 workload survey, half (49%) of GPs reported they are still working hours long enough to jeopardise patient safety.
An average 11-hour day including eight hours of clinical care, our 1,400 respondents told us, means they are dealing with 37 patients per day on average – far in excess of the maximum of 28 contacts they feel is safe during the pandemic.
Although patient demand did initially reduce at the outset of the pandemic, the pressures soared as staff fell ill with Covid, leaving fewer people to deal with completely reorganising practices and premises.
GPs also had to deal with more remote consultations. More than half (55%) of survey respondents tell Pulse this new way of working mean appointments are longer than before the pandemic.
Also, there are worries that it is easy to miss nuances about a patient’s condition, communicated through body language and facial expressions, which are often picked up when a consultation is conducted face to face.
Some 70% of survey respondents said workload was slightly or significantly higher since the pandemic began, with 40% saying they received more patient complaints. Seven million consultations were reported per week (January 2021), and one-third (29%) of consultations involving ‘very complex’ patients. There are also bottlenecks created by patients using E-consult over the weekend. The situation seems untenable and it’s no surprise that many GPs have been left contemplating their future in the profession.
One salaried GP told Pulse: ‘The pressures of the last 12 months have sharply brought into focus what is important. I’ve handed in my notice and chosen to prioritise my wellbeing. I’ve left a career I love as the emotional toll and impact on life outside work is too great.’
Cases like this are not rare, and GP burnout – together with failure to recruit doctors into general practice – are in part responsible for practices continuing to close throughout the pandemic.
Pulse conducted an investigation last April, which revealed 96 practices had shut across the UK, and a similar figure had the previous year.
Patients who are displaced as a result have to go somewhere, meaning nearby practices see their list sizes – and consequently demand and workload – increase. The circle becomes ever-more vicious.
According to Pulse columnist Dr Tony Copperfield, there are three options for tackling rising workload: divert the work; contain the work; and reduce demand.
None is easy or palatable, and all roads potentially lead to greater healthcare inequalities. Meanwhile, GPs continue to be collateral damage.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














