
The third game-changing development nominated by the RCGP is the digitisation of patient data. Former chair Professor Dame Clare Gerada looks back – and forwards
I have been a GP in the same south London practice since February 1991. When I started, a new GP contract had just been introduced. For the first time, GPs were paid according to activity in a few key areas, such as new patient health checks, childhood immunisations, vaccinations and cervical smears. This was a time of paper records, payment systems based on quarterly returns using cumbersome analysis of patient numbers, and manual paper searches of cards in a box that listed patients according to age, gender and the month or year to send a recall. This all took time.
Sometime in the middle of the 1990s, my practice manager announced we were switching away from paper. We’d keep paper FP10 prescriptions, letters and results, but everything else would be computerised. I asked, ‘But how can we tell if a patient is a frequent attender if we can’t see the weight of the notes? How will I remember what I felt if I can’t see what I have written in the margins?’ I feared that moving to fully electronic records would be a step too far.
How wrong I was. Adopting digital technology was a seismic change in how we could practise. We didn’t have to sift through pages of illegible handwriting to find out when and why a particular medication was prescribed. We could see who was coming, how often, who was not coming, and why not. We no longer had to rely on those clunky paper call-recall systems. We could conduct computer searches, which gave us much more accurate data on who to target for immunisation or who needed a cervical smear.
This allowed us to improve the efficiency of healthcare delivery, enhance patient care and streamline admin processes, including payments, appointment scheduling and patient registration. It led to the QOF, which led to more rationalisation and rigour in using disease codes to record patient findings and procedures.
Paradigm shift
Technology has brought a paradigm shift in how I have been able to work, and I have embraced new systems and innovations, whether that be a BlackBerry device or email. My practice developed the digital triage tool eConsult. It began as an idea one cold spring morning sometime in the 2010s. On the way to our usual 8am Monday partner meeting, we had all passed patients queuing for appointments. One colleague said: ‘I wish we knew what the patients needed before they came into the room; we could allocate proper time to them.’
Of course, 75% of patients did not need to see a GP, but we could not work that out until they were in front of us. We spent the meeting discussing how we could find out why the patient needed to see us. We talked about using email – but this was a non-starter as it would be too cumbersome and unsafe if scaled up beyond a few patients.
Over the next few weeks, we discussed creating a limited but robust set of digital templates for our website, which patients could fill in and give a history so that we could safely allocate them to the right clinician, with the right degree of urgency. eConsult was born.
Nearly a decade later, the pandemic catalysed the move to digital-first, which, despite the misgivings of some national newspapers, is a popular and far safer means of consulting for millions of patients every month. GPs can now care for patients remotely across the whole care pathway, from registration to consultation, investigations, referral, prescribing and follow-up. Of course, not every patient, condition or episode of care can or should be done remotely, but we have the technology available for those who wish to be seen in this way, and increasing numbers are choosing it.
And so to the future. We now have artificial intelligence and have to explore how to best use it. I have used ChatGPT and found it extremely useful when working on digital consultations before I respond to the patient. I recently undertook a blind assessment of AI versus a GP. I was asked to differentiate between the GP and the robot and give each a score. I identified all of them correctly, and the GP’s answers were marginally better. Nevertheless, the robot’s answers were acceptable. Just around the corner is AI that will not just support decision-making but will help diagnose and advise on treatment.
Embrace the power
We must learn AI’s power, not shy away from it. Each introduction of technology has faced negativity and reluctance, not from my patients but from the profession. While it’s right that our professional bodies, whether they are royal colleges or trade unions, are cautious about change, it’s also important that we all move with the times rather than hark back to a bygone era that was not perfect. Yet the future is coming ever faster. Patients have power in their hands, and we must ensure we move with the times as a profession and not create unnecessary obstacles.
A few years from now, all GPs will consult differently, using the same skills but working in a new way. Most consultations will start online, with a safe algorithm allowing the GP to capture relevant data and screen for red flags, and real-time patient indices such as blood pressure, pulse and oxygen saturation.
AI will sift consultations according to severity, conditions, urgency and patient choice. Digital consultations will be automatically directed to a relevant specialist. The GP will consult online, via video, and also face to face in person. Each consultation will be transcribed automatically into the medical notes, not as free text but arranged coherently.
AI will support the clinician’s decision by pulling data from the notes to remind the clinician that the patient presented with XYZ 10 years before, which might be relevant. The patient and clinicians will all have access to the electronic medical records, with the patient being the data controller. GPs will no longer refer patients for a second opinion. Instead, both patient and GP will have direct access to an appointment book.
All of this is possible today. We must ensure it is even better tomorrow.
Professor Dame Clare Gerada is a former chair and president of the RCGP
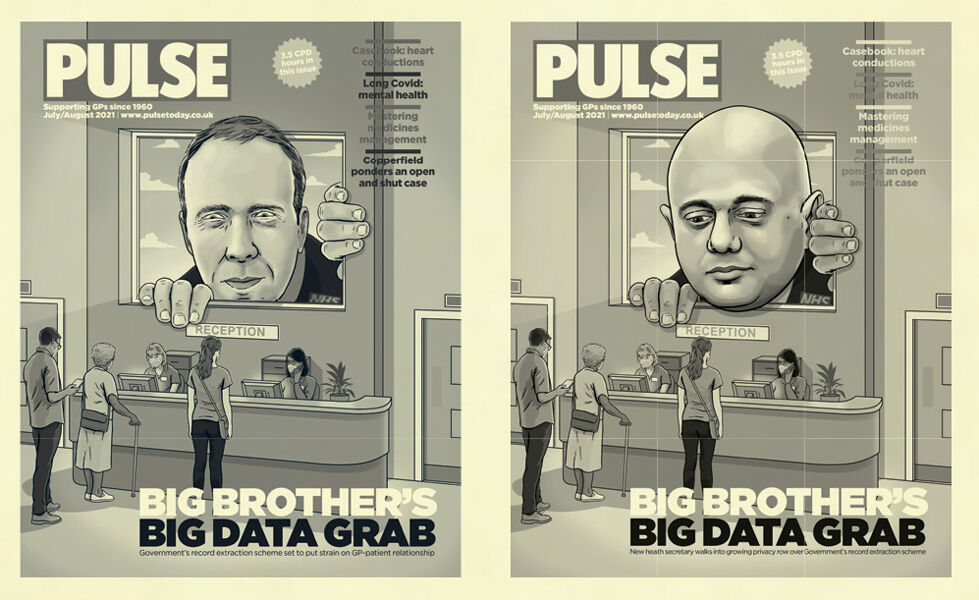
‘There is a darker side to the patient data issue, with various governments seemingly tempted to sell it to private companies. One such enterprise was the General Practice Data for Planning and Research scheme in 2021, which planned to extract data from GP systems. But the most memorable aspect of this story for me is the front cover. We sent the issue to press with Matt Hancock on the cover. And then, unfortunately (depending on your viewpoint), Hancock was sacked. After frantic calls to our art director James and the illustrator on a Saturday evening, I called the printer and fulfilled a lifelong ambition to shout “stop the press!” so we could replace Hancock with Sajid Javid.’ Jaimie Kaffash, editor, 2018-present


Digitising patient records has transformed our working practice and how we deliver care – it has allowed us to look for and act on trends in illness. To anyone accusing GPs of not moving with the times, this is an area where we have truly led the way! RCGP chair Professor Kamila Hawthorne on why the college chose patient data advances among its major developments in general practice


















For me, Professor Gerada has explained why parts of my job as a GP became dehumanised especially over the last 25 years. She has successfully painted a vision of the heartlessness of this new religion of Dataism (Homo Deus, Harari).
The predictable busy interference from AI in the consultation may render any chance of a meaningful and personal dr-pt encounter unattainable, and reduce the role of the GP to a sorry simulacrum of what we have been expert and wise at doing, reducing us to slavery to data and algorithms.
I’m put in mind of the scientists who discovered nuclear fission never once thinking it would lead to the making of the nuclear bomb. This Holocene Age we live in requires that we start being more circumspect in any change dressed up as progress. In this case, it would not be progress nor change but a mutation.
The dangers of Big Data have been recognised so I’m not breathlessly for it. Artificial Intelligence? How about Homo Sapiens exhausts Real Intelligence first? More informed debate is necessary.
*25 years* should read “10 years”
>25 years is my time as an NHS Dr
This is such a disappointing article from someone who wields so much influence. A few points:
1. I have to question the logic of your partners meeting being 8am on a Monday morning. No wonder the queue was so long.
2. The comment that remote digital consulting is ‘far safer’ than face to face. You might think it is just as safe as face to face care, but MORE safe? I struggle to see how that can be true.
3. AI has a long, long way to go before it is anywhere near ready to be used in the way described. Look at 111, an algorithm even with a human operator is risk averse and struggles with the nuances of a clinical presentation. Even now, most of the time chest pain = ambulance, regardless of other factors. It increases workload, it does not support the system. Do not get caught up in the romance of an AI driven utopia. I fear AI tools being forced on the system by those with influence, when they are not ready and only increase work.
Patients do like digital consults yes, but we must be careful not to confuse what patients like, with what is good medicine.
Example just from today – a patient had a video consultation with a private doctor for a testicular lump. Of course, he was told to see his GP. You might have thought it was obvious to the patient that digital was not appropriate for this problem, but he did not. This is how things go wrong.
When a chair of the RCGP (for goodness sake) believes this tosh I know we are done for.
Beyond awful