PMS practices could be forgiven for thinking ‘not again’. After years of managers chipping away at locally agreed contracts, GPs now face even more pain, with a sweeping NHS England review threatening up to £260m nationally – and possibly heralding the end of PMS altogether.
The two-year funding review was announced last month, after an NHS England analysis found PMS practices receive an average ‘premium’ of £14 per patient, with most of it not formally attached to any additional services.
The review aims to ensure ‘equality of opportunity’ for GP practices, and could mean a financial boon for GMS practices if funding is shared out more equally between practices via enhanced services.
But NHS England has not guaranteed that the funding will remain within general practice, and GP leaders warn that any benefit will be offset by GPs being asked to do more work to justify the additional funding and large numbers of PMS practices making the switch back to GMS.
Even the chair of the GPC, Dr Chaand Nagpaul, says he will consider switching his practice back to GMS, seeing little advantage in remaining on his locally negotiated contract.
‘For a large number of PMS practices that provide similar services to GMS, there will arguably be no benefit at all in remaining as PMS,’ he says.
The review comes amid declining numbers of PMS practices – there were 3,270 in 2012, down 45 on 2011. Plummeting earnings may be partly to blame. Figures from the Health and Social Care Information Centre show PMS partners’ income fell from an average of £113,400 in 2011 to £111,600 in 2012, a decrease of 1.6%. This compares with a 0.7% reduction in GMS partners’ income over the same period.
PMS practices have already suffered successive squeezes thanks to a programme of rolling ‘value for money’ reviews that began in 2006. A Pulse investigation last year showed that one PMS practice in three has had its contract changed since 2011.
NHS England insists its new review is needed to ensure that area teams ‘secure best value’ from the additional funding given to PMS practices. In a letter to area teams it stipulated that PMS contract reviews must reflect local strategy for primary care, secure services above and beyond GMS and help to reduce health inequalities (see box, below).
It added: ‘It is essential that we apply the principles of equitable funding by moving towards a position where we can demonstrate that all practices (whether GMS, PMS or APMS) receive the same core funding for providing the core services expected of all GP practices.
‘Any additional funding above this must be clearly linked to enhanced quality of services or the specific needs of a local population, and practices should have an equal opportunity to earn premium funding if they meet the necessary criteria.’
In a white paper in 2010, the coalition Government set out its aim for a single contractual mechanism for all practices. This now looks unlikely, as NHS England says it remains committed to retaining PMS contracts, albeit after bringing practices down to the same level of core funding. The King’s Fund and the Nuffield Trust recently recommended that GPs be offered a new, additional contract alongside GMS and PMS contracts to encourage them to federate and integrate with other community services.
GP dismay
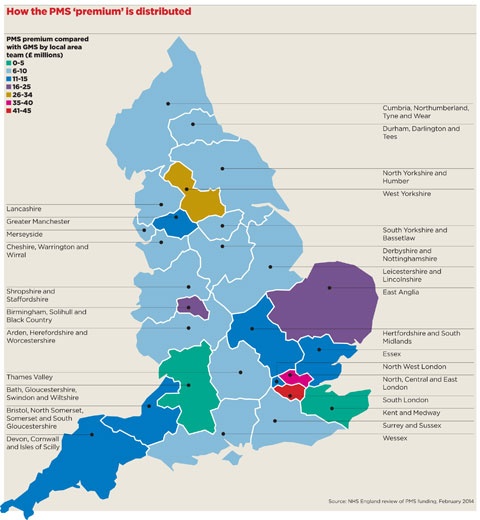
Practices in London and northern England look set to be hit hardest by the review, as they benefit most from the so-called PMS ‘premium’ (see map, page 28). However, local area teams have been given flexibility over the timetable for reallocating funding and have been told to involve LMCs in the process.
Practices that have had a recent review of additional funding may be exempt but by March 2016, all PMS practices will have to move to a ‘model PMS contract’.
PMS GPs have responded with dismay. Dr Peter Smith, a PMS GP in Kingston-upon-Thames, south-west London and vice-president of the National Association of Primary Care, describes the guidance as ‘one of the most catastrophic, ill-thought-out documents to have emanated from any NHS executive for the past 20 years’.
He adds that there is ‘no guarantee’ in the document that PMS practices will get to keep any of their funding for additional services, and warns the pace of change could cause problems for many.
‘If area teams decide to go for a much faster transition, it will definitely destabilise many practices. Locally, a couple of practices have already closed because of PMS reviews,’ he says.
‘We lost 13% of our funding in a PMS review three years ago. If the local area team decides to do something similar again, and to push this through over just a two-year period, that will destabilise us.’
Death knell?
Some GPs are unconcerned. Dr Jane Lothian, medical secretary of Northumberland LMC and a PMS GP in Blyth, thinks the forthcoming review ‘won’t really affect’ her practice as earlier reviews have already stripped away most of the additional funding. ‘If they did review it, all they would get from us is a few pence,’ she says.
But a founding father of PMS wonders if the contract may have died years ago.
‘I don’t know if I missed the passing of PMS,’ says Dr James Kingsland, a GP in Merseyside who was the Department of Health’s clinical adviser when the PMS pilots were launched in 1998.
‘PMS was set up because the Government at the time recognised that by moving more services into primary care you could reduce admissions, urgent care needs and long-term condition management in hospital. And it worked.’
But the latest review of PMS funding may be the last straw even for Dr Kingsland: ‘You ask why we are still a PMS practice. The answer is – I don’t know.’

Dr Chaand Nagpaul: ‘It is inevitable some will switch to GMS’
I don’t have any idea how this review will pan out. We hope area teams will be fair and not use PMS as a ‘soft target’. But we are worried they will take this money away and use it to plug other gaps. We believe this money should be redeployed to GP surgeries and not used for other purposes, like offsetting deficits in other parts of the budget.
It is inevitable that some practices will switch to GMS, because on the lower end of the scale it will make little sense to remain PMS if reverting gives them the equivalent or better funding. It is something I would consider for my own practice.
There will always be a need for PMS, but for a large number of practices that provide similar services to GMS, there will arguably be no benefit at all in remaining as PMS.
Dr Chaand Nagpaul is chair of the GPC and a GP at a PMS practice in Stanmore, north-west London
What will the review entail?
NHS England has told area teams to review the use of £260m of PMS funding over two years from 2014. Additional funding given to GP practices above core national requirements must:
• Reflect the local primary care strategic plan (as set out by area teams/CCGs).
• Secure services, or outcomes, above and beyond GMS contractual terms or improve premises, ‘for example, to support delivery at scale’.
• Give ‘equal opportunity’ to all local GP practices, including GMS.
• Reduce health inequalities.
Area teams should also:
• Involve LMCs in discussions about how money is reallocated.
• Prioritise contracts with the largest premium per head, or those that have not been reviewed recently.
• Ensure all practices are shifted to a common PMS contract.
Source: NHS England letter to area teams, 2014
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














