As the demand for mental health services grows, NHS England has funded a regional pilot project led by Dr Miranda Budd and her GP colleagues in the North-West to create placements for GP trainees in mental health settings. Following its success, the team now proposes that other regions do the same
The GP is usually the first port of call for those seeking mental health support, and it is estimated that around one in three GP appointments involve a mental health component.
However, there has been a growing concern that GP trainees are not adequately trained to provide mental health care in their future workplace. Last month, GPs and other staff working in primary care were asked to take part in a public consultation on the skills needed to respond to patients with mental health needs as the national demand for mental health services increases.
What’s more, a 2016 report by the mental health charity Mind found that less than half (46%) of GP trainees undertook a training placement in a mental health setting. The only mental health-related option offered to them was in psychiatry, which relates to secondary and tertiary care. As a result, Mind has recommended all GP trainees to undertake a placement in a mental health setting and questioned the ability of placements in secondary and tertiary care to appropriately equip them to work in primary care.
While there is no doubt that a rotation in psychiatry can be helpful for GP trainees, there are other settings – particularly those providing primary care mental health services, such as NHS Talking Therapies, for anxiety and depression – that could be used to provide more relevant learning experiences.
NHS England has outlined its vision for transforming GP Specialty Training in its Training the Future GP report, which highlights the importance of ensuring the future GP workforce is well equipped to manage the presenting mental health need. The report, published in March 2023, proposes that having an enhanced awareness of mental health issues within primary care is paramount going forward.
In an effort to realise its vision, NHS England has been supporting a pilot project to set up and support integrated training posts in the North-West, which are split between general practice and NHS Talking Therapies. The project aimed to understand the feasibility of such posts and produced a framework to enable more of them in primary mental health care services in the North-West and beyond.
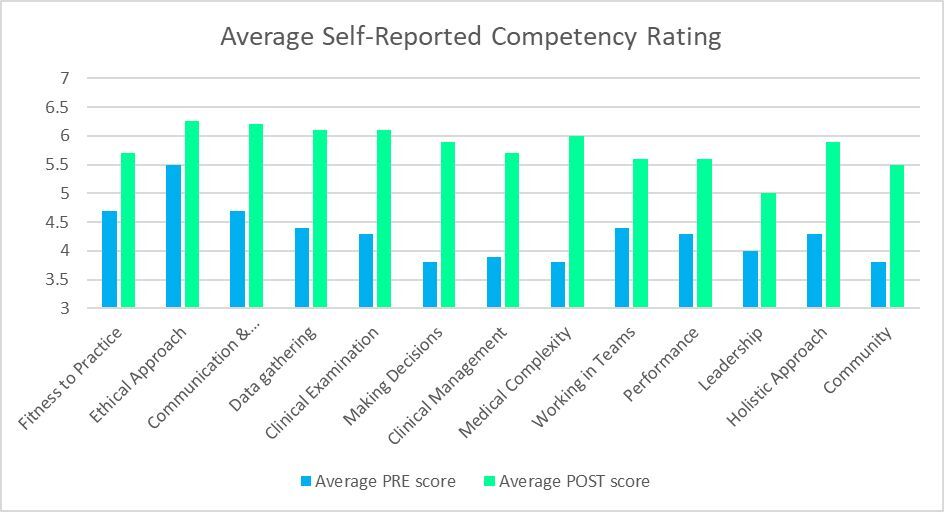
After scoping interest from North-West GP training programmes and NHS Talking Therapies, four integrated training posts were developed – three in Greater Manchester, one in Lancashire – and ran between February and August 2023. Although lessons were learned along the way, the programme proved to be a fantastic learning opportunity for GP trainees, with their average competency scores improving in all 13 areas over the six-month period (see below).
Meanwhile, feedback from the trainees, supervisors and NHS Talking Therapies staff was positive, too. Some of the key themes related to the skills and confidence the trainees developed through enhanced understanding about mental health advice and NHS Talking Therapies, which included service remit and suitable patients. Furthermore, trainees were able to provide a better explanation of available support to their patients in general practice and had the opportunity to share what they learned with other GP colleagues. Trainees also reported a positive impact on their own mental health.
That said, there is a need for greater clarity in relation to the GP trainee’s role and remit, as well as their understanding about the current level of skill in psychological ways of working. Workforce and capacity issues within NHS Talking Therapies meant that supervising an additional other put pressure on the service, and there was a need for clear communication from the start between all supervisors.
In addition to the above, some NHS Talking Therapies services raised an issue about how the clinical activity delivered by the trainees would be recorded. Within NHS Talking Therapies there are guidelines in relation to recovery data and the need to be an ‘approved clinician’ or having completed an NHS Talking Therapies-specific training course to be able to work with clients and the data counting towards set targets. This topic needs discussing further within NHS England to reach a clear solution.
There is still a lot of work to be done, but thanks to the pilot programme’s success, we have managed to set up other integrated training posts across the North-West. Going forward, we can only hope it will support others elsewhere to create similar posts, too.
Dr Miranda Budd was a consultant clinical psychologist within Lancashire and South Cumbria NHS Foundation trust while leading the project funded by NHSE; Dr Nick Walton is NHSE’s associate dean for Bolton, Salford and Trafford GP training schemes; and Dr Bob Kirk is NHSE’s primary care dean
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













This sounds like a slide to getting GP’s providing talking therapies and not properly commissioning the service. I would be hesitant in the extreme in going down this line with trainees in primary care health settings to essentially learn CBT and other talking therapies.
are we saying that GP trainees in Psychiatry SHP posts are not being given good quality training by their CMHT/Consultant Psychiatry colleagues?
What does the Deanery GP VTS inspectorates say about this poor quality of job experience? Should they make directions or remove post approvals?
So, more training——–after five years at medical school and a years probation—— did we end up being competent in anything?
Exposure to mental health is already part of training. As is exposure to menopause, child health and all the other poorly commissioned aspects of health that the government is failing the public on.
The problem is not with training of GPs but with provision of mental health services.
I really don’t understand this one bit
If 1 in 3 presentations to general practice is mental health related, then surely the best placement for trainees is….general practice.
How is an attachment to talking therapies going to enable you to assess, identify red flags, diagnose, and treat (then document) in a 10-15 minute consultation?
We don’t really want trainees to adopt a lengthy CBT approach to mental health issues – that’s not our role or what we are funded to do.
DOI: intercalated with a psychology BSc and started out in a psychiatry career
Psychiatry was probably the most useless of the rotations we endured; though the magnificent work-avoidance skills of some of the consultants was no doubt inspirational for some. Geriatrics, A/E, Paeds far more useful.
Disagree with this on many levels. The majority of mental health presentations to primary care are NOT with a mental health disorder. The majority are low level issues with emotional regulation, resilience, environmental stressors such as housing, jobs, relationships etc. None of this is “medical”. And none of this is well dealt with by anybody in a 10 minute appointment.
The only upshot of medical presentation is an exccess of antidepressant prescribing, the majority of which is unnecessary at best and potentially harmful at worst.
Rather than the usual battle cry of “GPs need more training” we should be pushing to say that this is not medical, should not sit in primary care and pushing for direct patient access and/or signposting to Talking Therapies/social prescribing, VCS partners, CAB, etc.
Once low level distress/anxiety/low mood etc has passed a threshold to be classed as true psychopathology then indeed it becomes medical, but by filtering the high volume/low intensity subset of presenting patients into more appropriate services we free up time to be spent on those more appropriate to OUR skillset as medics rather than expecting medics to also become CBT/DBT/ACT/mindfulness expert psychologists.
Carpe Vinum – Thank you!