Analysis: GPs take the strain of ‘Austerity Britain’

The triple whammy of public spending cuts, welfare changes and the after-effects of the recession means practices are increasingly finding themselves managing the repercussions of ‘Austerity Britain’.
Whether it is referring patients to food banks, supporting their benefits appeals or helping them to cope with soaring levels of stress and anxiety, many GPs are now being confronted with ballooning social issues on a daily basis.
And with the introduction of a new disability payments system, and Chancellor George Osborne targeting a further £25bn in spending cuts after next year’s general election, worse could be to come.
Dr Andrew Mimnagh, a GP in Sefton, Merseyside, says the additional workload resulting from social problems is becoming ‘ridiculous’.
‘My staff are spending a lot of time on this and a lot of booked appointments turn out to be patients expressing dissatisfaction about their [benefits] claims,’ he says.
As an example of this trend, Dr Mimnagh cites the ratio of appointments about mortgages and personal medical attendance reports to those about benefits, which, he says, ‘has exactly reversed since the height of the boom’.
‘In the good times, it was 80% mortgages and PMAs, 20% benefits. Now it’s 20% mortgages and 80% benefits,’ he says.
Huge rise in requests
Figures obtained by Pulse under the Freedom of Information Act last year indicated a 21% increase in Employment and Support Allowance (ESA) requests to medical professionals – the majority GPs – on behalf of the Government in the first three months of 2013, compared with the previous year.
Now new Department for Work and Pensions (DWP) figures obtained by Pulse reveal that, between September 2013 and February 2014, ‘medical practitioners’ were asked for additional medical evidence by DWP contractor Atos for a third of incapacity and ESA claims – some 305,533 cases in total.
A DWP spokesperson says requests for additional evidence are sent to GPs when face-to-face assessments are ‘clearly unnecessary’, adding: ‘Claimants can also submit evidence in support of their claim at any point in the process.’
There was a furious row last year when the Black Triangle campaign group threatened legal action after several LMCs advised GPs to ‘just say no’ to patient requests for evidence to support their benefits appeals.
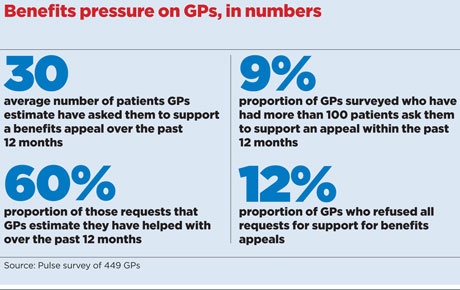
That legal threat was later dropped by the Black Triangle campaign in favour of working more closely with the BMA. But in any event, a Pulse survey of 449 GPs across the UK indicates practices do support the majority of requests.
GPs responding to the survey said they had, on average, supported 60% of requests for additional help from patients over the past 12 months. Around 10% of respondents said they had been asked to help patients more than 100 times over that period.
Despite many GPs’ willingness to help their patients, figures released by the DWP in November 2013 showed that GP evidence was the deciding factor in only 2.9% of benefits cases.
And GPs now say the pressure is becoming intolerable and is affecting the doctor-patient relationship. Dr Robert Morley, executive secretary of Birmingham LMC and a GP in the city, says: ‘GPs are being asked to provide specific letters – sometimes appropriately, sometimes not – which can cause difficulties in consultations.
‘These sorts of requests are certainly worse in the past year or two. It’s a combination of the recession generally and the Government’s welfare cuts.’
Disability changes
The introduction of the new Personal Independence Payment (PIP) is already proving to be another headache for practices. It was brought in as the replacement for the Disability Living Allowance nationally from June 2013 and the GPC says it is concerned about the way it is being rolled out.
A PIP is given only after an independent assessment of a claimant’s ability to complete daily tasks. GPs are paid £33.50 per patient to give details of their diagnosis, history and treatment, and the impact of the disabling condition on the patient’s life.
The new system is supposed to save £3bn in benefits spending by 2018-19, but Dr John Canning, chair of the GPC’s professional fees and regulation committee and a GP in Middlesbrough, says practices could be hit by yet more requests for help when PIP assessments are appealed.
‘There should be no presumption that doctors can work for nothing,’ he says.
There are some signs, though, that the Government is beginning to recognise the burden on GPs, with its new Health and Work Service due to be up and running by the end of this year.
Under the scheme, which will be run by the private sector, employers or GPs will be able to refer people who have been off sick for more than four weeks for non-compulsory medical assessments and treatment plans – a move which could alleviate some of the current burden on GPs.
Unemployment
GPC deputy chair Dr Richard Vautrey, who practises in Leeds, says that he has also noticed the impact of a very difficult jobs market in his surgery waiting room.
‘The challenge of unemployment is a particularly big one, especially for young people,’ he says. ‘They are presenting more and more because of stress and anxiety – normally you wouldn’t see young people in most GP surgeries.’
Related articles
Sickness and disability benefits (1 CPD hour)
Some patients are even struggling to pay for prescriptions, he adds. ‘Patients are reluctant to tell us and it’s only later that we’ll find out they haven’t been taking their medicine because they couldn’t afford it.
‘People will also sometimes ask you to print out separate prescriptions, as they can only afford to get one at a time. There are quite a few people caught in the trap of low-paid jobs where they don’t qualify for exemptions.’
‘Buckling under’
A Pulse survey published last month found that as many as one in six GPs has been asked to refer a patient to a food bank within the past 12 months.
Food bank charities are increasingly requiring a referral from a sanctioned support agency, which can include schools, GPs or the jobcentre, to ensure that support ends up reaching the most needy.
And it is this type of additional work, often unfunded, that is crippling practices, says Dr Nigel Watson, chief executive of Wessex LMCs and a GP in the New Forest.
He says: ‘It’s not unusual in surgery to have half a dozen patients who don’t actually need to see you. They might be consulting to change a referral under Choose and Book or they might need to see a social worker or their benefits have been cut and they don’t know what to do.
‘In the end, it’s the straw that breaks the camel’s back. There are lots of really good practices trying to go the extra mile for patients that are buckling under the strain and about to implode.’
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













