
NICE guidelines are seemingly becoming increasingly detached from day-to-day general practice.
In key areas of primary care – cardiovascular disease, diabetes, asthma, cancer diagnosis – the latest guidance from the institute has been criticised by experts and grassroots GPs.
Recent draft guidelines have met with incredulity from GPs, with diabetes recommendations described as ‘bonkers’, asthma diagnosis advice as ‘dangerous’ and cancer referral instructions as ‘overwhelming’.
NICE has found itself in direct and public conflict with the BMA over its statins advice and former NICE members have told Pulse that the detachment from primary care is getting worse, with GPs ‘marginalised’ on NICE panels.
This all comes as the Labour party tells Pulse it is considering setting ‘tougher rules’ on implementing NICE guidelines if it is elected in May.
NICE has said it is looking to tailor guidance towards primary care, and is set to start work on ‘multimorbidity’ guidelines that will be more attuned to the care that GPs give.
But its most recent major guidelines have failed to chime with the realities of primary care.
As Dr Nick Summerton, a GP in East Yorkshire and former NICE adviser, puts it: ‘The guidelines have always been a bit remote and they’re getting worse.’
A draft update of the type 2 diabetes guidelines, released in January, has proved to be among the most controversial in years, recommending an overhaul of the treatment algorithm for glucose-lowering as well as the use of repaglinide as an alternative first-line therapy in people who cannot tolerate metformin.
‘Nonsensical’
The recommendations – but especially the use of repaglinide – have variously been described by experts as ‘bonkers’, ‘outrageous’, ‘nonsensical’and as having the potential to ‘set back modern diabetes management by decades’. Most alarmingly, Dr Adrian Brewster, a GPSI in obesity and Type II diabetes in Reading, says: ‘This makes a laughing stock of NICE – this is not clinical excellence.’
In the same month, the draft guidelines on asthma diagnosis recommended a battery of new diagnostic tests such as exhaled ferrous nitric oxide (FeNO) breath tests and bronchial challenge tests – none of which is routinely available in either primary or secondary care – to address what NICE claims is a 30% overdiagnosis rate for the disease.
But experts say NICE’s overdiagnosis figures are ‘misleading’, with one respiratory expert even calling the media coverage resulting from NICE’s press release ‘dangerous’. They also have ‘huge implications’ for GPs and are at odds with newly revised asthma guidelines issued by the British Thoracic Society (BTS) and Scottish Intercollegiate Guidelines Network (SIGN), which urged GPs to take a more pragmatic approach involving trials of treatment.
Meanwhile, draft guidelines for suspected cancer published in late 2014 have been described as too complicated and unwieldy for GPs to use in daily practice, and the authors of a Cochrane Review told Pulse they were ‘perplexed’ that NICE was continuing to recommend antivirals for either the treatment of flu or for a prophylaxis, despite evidence suggesting a lack of efficacy and concern over side-effects.
‘NICE has very little relationship with my world’
Dr Peter Swinyard, chair of the Family Doctors Association
Draft guidance on antibiotics released last month that suggested GPs should be given annual reports on their antibiotic prescribing and local resistance patterns, were denounced for increasing bureaucracy.
The advice was also branded ‘pointless’ when the National Association of Sessional GPs pointed out that locums often prescribe under other doctors’ names, as they do not have prescriber codes, meaning that the reports could do more harm than good.
The torrent of criticism comes with NICE still reeling from the controversy over its decision last year to halve the primary prevention risk threshold for statins treatment to 10%.
At the time, many GP leaders warned this would lead to over-medicalisation and a Pulse survey last year showed two-thirds of GPs were ignoring the advice.
The row flared up again last month after it was revealed the researchers responsible for the work endorsing NICE’s recommendations had decided to issue a call for unpublished statins safety data to update their calculations.
The Cholesterol Treatment Triallists (CTT) group has requested all available information on side-effects from trials of statins – including so-far unreported data from other trial investigators – although NICE argues that this analysis is unlikely to change its recommendations.
Better GP representation
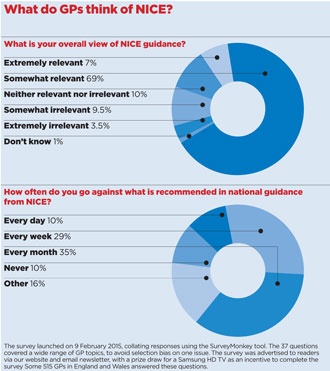
A Pulse survey of 515 GPs reveals that although the vast majority of English and Welsh GPs believe NICE guidelines are at least ‘somewhat relevant’ to their practice, more than 70% admit to departing from NICE recommended practice at least once a month and 10% say they do so on a daily basis. But Dr Summerton believes the disconnect between GPs and NICE will intensify, and stems from a lack of GP representation, which itself is a consequence of the failure properly to reimburse GPs who sit on guidelines committees.
NICE says it is making moves to try to connect with GPs.
Under the chairmanship of former GP Professor David Haslam, the institute is reviewing how to make the guidelines more GP-friendly. He insists NICE is putting GPs at the heart of its work.
He tells Pulse: ‘We are developing guidelines on multimorbidity, we are working on how best to help shared decision making with patients, and we are looking at how best we can provide rapid access to information for busy GPs.
‘Guidelines, must be deliverable by GPs within the available resources’
Dr Andrew Green, chair of the GPC’s clinical and prescribing subcommittee
‘As someone who spent 36 years in frontline general practice, I absolutely agree that it is essential that GPs are closely and realistically involved in NICE.
‘Indeed, from sitting on our committees to advising on the development of our guidance, GPs absolutely play a central role.’
Professor Haslam also defends the basis of the institute’s work, and insists that it is underpinned by input from primary care.
He says: ‘NICE has produced several resources to help GPs use its guidance and find out about the evidence that underpins our work. Data is gathered by expert analysts and assessed by our independent committees (including GPs) who have the skills and experience to interrogate the evidence and develop robust guidance of relevance to the NHS – and primary care.’
Dr Andrew Green, chair of the GPC’s clinical and prescribing subcommittee, says the GPC is working with NICE with a view to providing more appropriate guidelines.
He says: ‘We believe that it is vital that the guidance NICE produces is not only academically valid but is also accessible, concise, relevant, and above all deliverable by GPs within the limitations of the resources available.
‘We do have meetings planned with NICE to explore how we can work together to achieve these aims.’
Reimbursement
NICE has attempted to address the issue of GP reimbursement – the main criticism voiced by Dr Summerton. Internal locum cover is now reimbursed up to a maximum of £350 per day, up from £300 in December 2013, and where an external locum agency is used, a practice can claim up to £500 per day, up from £400.
But Dr Rubin Minhas, a GP in Kent and former lipid guidelines adviser who also chairs the BMJ ethics committee, worries this is not enough and the difference in fees for internal and external locum cover demonstrates a lack of awareness from NICE about general practice.
Dr Minhas says: ‘No partner would work for less in their own practice when they could be getting more down the road as an external locum. It is a bit disappointing as NICE… doesn’t seem to have much of a handle on what GPs are doing.
‘Their policy basically marginalises GPs from being involved while their guidance is increasingly skewed to secondary care.’ Dr Peter Swinyard, chair of the Family Doctor Association, agrees NICE is becoming detached. He says: ‘NICE seems to work in some extraordinary environment which has very little relationship with the world in which I practise.’
Unfortunately for GPs, rows over the guidelines are not simply academic. Pulse understands that Labour intends to set up a ‘wide-ranging review’ into the way NICE guidance is implemented if the party is elected into government in May, to establish ‘tougher rules’ on how it is applied in the NHS.
A spokesperson for the party told Pulse: ‘Specifically, the review will look at whether there should be a more robust approach to implementation of NICE guidance and appraisals, and if should there be a requirement on commissioners to report and explain any departure from NICE guidelines.’
Elsewhere, the QOF advisory committee is currently consulting over putting the 10% 10-year CV risk threshold into the framework, despite deep reservations among many GPs.
Dr David Jenner, a GP in Devon and chair of the Eastern and Mid-Devon locality of NHS Northern, Eastern and Western Devon CCG, explains: ‘NICE has been good in many ways and GPs can, of course, interpret the guidance and discuss its relevance with patients. The problems arise when it is made mandatory through QOF.’
If this all comes to pass, their increasingly detached nature will be anything but a joke for GPs.
New NICE guidelines
Cancer (draft)

What does NICE recommend?
There are 47 new recommendations, including urgent referral of 40- to 55- year-olds who have never smoked for suspected lung cancer if they have haemoptysis (with other symptoms like fatigue or weight loss), and anyone over 40 with unexplained weight loss and abdominal pain for suspected colorectal cancer.
What did the experts say?
Dr John Hughes, former Manchester LMC secretary and a GP in the city, said: ‘It almost devalues training. If everyone with “x” symptoms has to be referred, then a clerical person could do it.’
What is the latest?
Consultation is now closed. NICE is considering responses.
Asthma diagnosis (draft)

What does it recommend?
‘Objective’ testing for asthma, including spirometry, bronchodilator reversibility tests and exhaled ferrous nitric oxide (FeNO) breath tests. Bronchial challenge tests are recommended in cases where there is uncertainty over the asthma diagnosis.
What did the experts say?
Dr Stephen Gaduzo, chair of the Primary Care Respiratory Society, said: ‘This will have huge implications for us, in terms of equipment, training, education, workforce and time.’
He described NICE’s claim that 30% of people having treatment may not actually have asthma as ‘dangerous’.
What is the latest?
Guidelines are out for consultation.
Type 2 diabetes (draft)

What does it recommend?
An overhaul of the treatment algorithm for glucose-lowering, as well as the use of repaglinide as an alternative first-line therapy in people who cannot tolerate metformin.
What did the experts say?
Dr Andrew Brewster, GPSI in obesity and diabetes in Reading, said the guidelines are ‘outrageous’ and risk making NICE a ‘laughing stock’.
Professor Roger Gadsby, a GPSI in diabetes, said many experts had called the repaglinide advice ‘bonkers’, while an editorial in the British Journal of Diabetes and Vascular Disease said the guidance would ‘set back modern diabetes management by decades’.
What is the latest?
The guidelines are out for consultation.
Lipid modification (final)

What does it recommend?
Halving the 10-year risk threshold for primary prevention to 10%, potentially leading to GPs putting millions more healthy people on statins.
What did the experts say?
The GPC warned the change would divert precious resources into treating healthy people at the cost of more needy patients. Former RCGP chair Professor Clare Gerada warned that the recommendation could lead to ‘over-medicalisation’.
What is the latest?
The recommendation was pushed through and in January 2015, NICE recommended adding the 10% threshold to the QOF. Last month saw accusations that vital safety data had not been published, undermining GPs’ confidence in prescribing statins to healthy patients.
Antimicrobial stewardship (draft)

What does it recommend?
Draft NICE guidance says local ‘antimicrobial stewardship teams’ should review GP antibiotic prescribing and provide individual reports to GPs to slow the development of drug resistance.
What did the experts say?
Dr Peter Swinyard, chair of the Family Doctor Association, says: ‘None of us is prescribing for fun and for NICE to say we should start sneaking on each other is quite bizarre.
‘I’m afraid the lack of understanding of what actually happens in consultations displayed in this guidance is mind blowing.’
The National Association of Sessional GPs, which represents locums, says: ‘It doesn’t look like NICE quite appreciates the issues’.
The association points out that locums do not have prescriber codes so scripts are often coded to other GPs in the practice – which would render the stewardship reports meaningless.
What is the latest?
The guidelines are out for consultation.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.

















