When the Prime Minister announced a £50m pilot to test seven-day, 12-hour GP access last October, many GPs hoped this pie-in-the-sky idea would quietly go away.

But just a year later, David Cameron has declared that pilot a ‘great success’ and announced a £400m investment to roll out the idea across England if the Conservatives win next May’s general election.
But quite how practices will provide this level of extended access on barely £200 per week of additional funding – and in the midst of a GP recruitment crisis – is not yet clear.
The funding will be spread over five years and only designed to meet ‘set-up costs’ so it is unclear if it will be recurrent.
But one thing is clear. With this level of funding, not every practice will be working an 84-hour week.
‘This is essentially funding to allow GPs to form federations’
Health Secretary Jeremy Hunt
Health secretary Jeremy Hunt told the RCGP conference this month that the proposal would not necessarily mean patients would be able to access their GP, their practice or even a face-to-face appointment. ‘I want to stress this is not a commitment that you will be able to see your own GP 24-7. GPs, just like politicians, need a break and it is not that commitment,’ he said.
‘This is essentially funding to allow GPs to form federations so people will be able book evening and weekend appointments – maybe not at their own surgery, maybe at a neighbouring surgery, maybe not face to face, maybe by Skype or telephone.
‘Patients may or may not be speaking to their own GP, but what they will be doing is speaking to a doctor who can access their medical record. I think it will be fantastically good for patients and will also help GPs and surgeries to work together.’
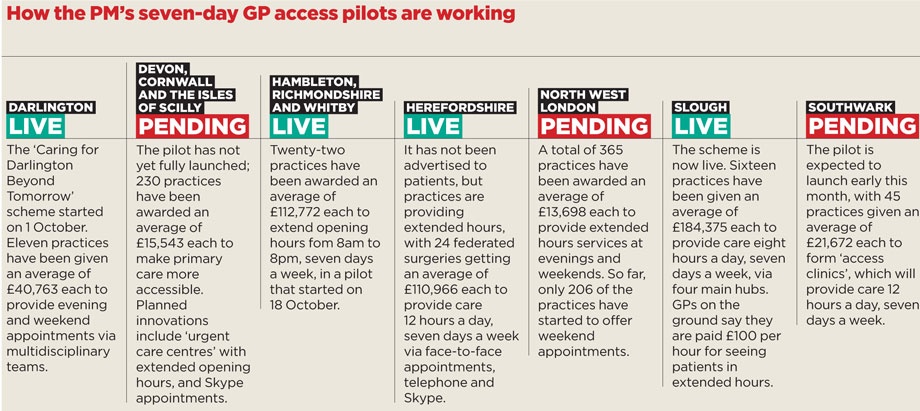
This fits the model of many of the PM’s pilots, which were announced at the Conservative party conference last year.
The model often involves federated groups of practices working in ‘hubs’ or ‘clusters’ sharing the provision of evening and weekend cover. But despite Mr Cameron’s upbeat assessment, many of these pilots have struggled to get off the ground.
In September, Pulse contacted seven of the areas given funding from April to open seven days a week. Only two could confirm they had started extended GP opening. A number of the others have since gone live, but this is a poor record when NHS England originally said they should start to go live in May – and the funding is set to run out next April.
The schemes that have gone live report stellar patient feedback. GPs in Slough, Berkshire, were given nearly £3m for extended access. Pulse has learned that the 16 practices running the scheme are paid £100 per hour and that evening and weekend appointments are exceptionally popular.
Positive response
Dr Jitendrakumar Trivedi, a GP in Slough, says: ‘Every appointment on my weekends is completely booked up, and the same probably applies to other GPs in the area. I see it as a positive thing – it will reduce my burden on weekdays.’
Herefordshire, too, has seen some success with its £2.7m pilot. Although it has yet to publicise seven-day access to patients, all 24 of its practices have been running extended hours in a three-hub system since the summer, with practices able to share patient records and access them with consent.
‘The scheme is sustainable only if you can find GPs who want to work seven days’
Dr John Rawlinson, chair of Berkshire LMC
The pilot has had a ‘really positive response’ so far, according to Dr Richard Dales, medical secretary of Herefordshire LMC and a non-executive member of Taurus Healthcare, the provider arm of Herefordshire’s GP federation. He says the federation is looking at expanding to cover emergency cases.
He says: ‘We are not far off full capacity now, but we have not publicised the scheme to patients. But I have no doubt the demand is out there. It is just a question of practices and patients getting used to it.’
But Pulse has learned that the projects in north-west London, Southwark, North Yorkshire, Darlington and south-west England have either just started or not yet begun. And the schemes in Herefordshire and Slough do not enjoy universal support among local GPs.
Dr John Rawlinson, chair of Berkshire LMC, tells Pulse: ‘It’s not about the money, it’s the workload. We’re overworked and under-resourced.’ He worries that the pilot scheme may soon take its toll, particularly because there’s no way to guarantee that patients can see their own GP seven days a week.
‘The scheme is sustainable only if you can find GPs who want to work seven days,’ Dr Rawlinson says.
Is seven-day access deliverable?
Yes
Recruitment issues are difficult here, as they are in many areas, and one of our biggest worries was whether we could attract enough GPs to do the work. But we’ve had a really positive response. We’re not far off full capacity now and we haven’t publicised the scheme to patients. I’ve no doubt that the demand is out there: it’s just a question of practices and patients getting used to it.
We have all three of our hubs up and running. Compared with other areas, we’ve done exceptionally well. The IT was the biggest worry, but the system is working well now. We have a robust data-sharing agreement with the practices.
Data protection is a tricky area, but we have a very clear contract between the practices and the patients to ensure data is shared correctly. We’re currently building our capacity and working with NHS 111 and A&E, so we’re able to see emergency cases too. We can currently see emergency patients as temporary residents, but we don’t have access to their notes.
Dr Richard Dales, medical secretary of Heredfordshire LMC
No
Not only is seven-day access just not possible on the available resources, but the worry really is this – where are the doctors? The young guys just don’t want to come into general practice at the moment.
The recruitment crisis is critical, and it’s been exacerbated by the pension changes that mean doctors are retiring much younger.
How on earth Jeremy Hunt has conjured up more than a million happy customers for this pilot scheme, I don’t know.
The pilot scheme in Watford hasn’t even properly got off the ground – sorting out the administration has proved to be extremely complex.
Even when it’s fully up and running, it will cover a miniscule number of patients, fewer than half of the population.
I’m told they’re filling the slots with some difficulty, but to the detriment of the out-of-hours service.
I’ve heard a certain exasperation from the people who have spoken to me about the scheme.
Dr Peter Graves, chair of Bedfordshire and Hertfordshire LMC
Sourcing staff to cover extended access in the middle of a national GP recruitment crisis is likely to be a problem for many areas, should seven-day access be rolled out across the country. In Slough, the burden of responsibility has fallen on the shoulders of GP partners. Dr Gurdip Hear is a partner at one of four Slough practices that hold clinics in extended hours. He says patients ‘love the scheme to bits’, but that staffing is the biggest problem: ‘The salaried and junior GPs aren’t coming forward to do this work, so it is the partners doing most of the extended hours cover.
‘Is it sustainable working for 11 to 12 hours a day, Monday to Friday, then working eight to 16 hours at the weekend? Time will tell.’
Another headache has been finding practice nurses and reception staff to work extended hours, and GPs have also begun to notice the pilot’s effect on the availability of locums. Some have also expressed concern over the potential impact on out-of-hours services, which in many areas are provided by the same doctors who will be asked to cover extended hours. According to Dr Rawlinson, many are finding it hard to tell the difference between seven-day access and ‘a better-run out-of-hours’.
Inadequate funding
This month, a group of more than 100 GPs wrote an open letter to Mr Cameron highlighting the discrepancies between the funds allocated to the pilot scheme and those purportedly ringfenced for its roll-out across the country.
Signatories to the ‘Resilient GP’ group’s letter told the PM: ‘This equates to a 1.1% increase in primary care funding for a 60% increase in workload.’
They added: ‘Do the maths, as your advisers obviously can’t. Forget the rhetoric and the arguments about doctor salaries, this fairy tale is simply not deliverable.’
Bedfordshire and Hertfordshire LMC chair Dr Peter Graves describes the funds allocated to the project as ‘ludicrous’. He says: ‘If £50m has allowed only nine sites to roll out seven-day access, how on earth can £400m over the next five years cover the rest of the country? We clearly need well over £1bn to do this.’
But the idea is not going away. A report from the London mayor – published last month and authored by former health minister Lord Ara Darzi – recommends a £1bn investment in London GP practice premises, on the condition they open from 8am to 8pm.
The extended access genie is unquestionably out of the bottle.