No room at the practice
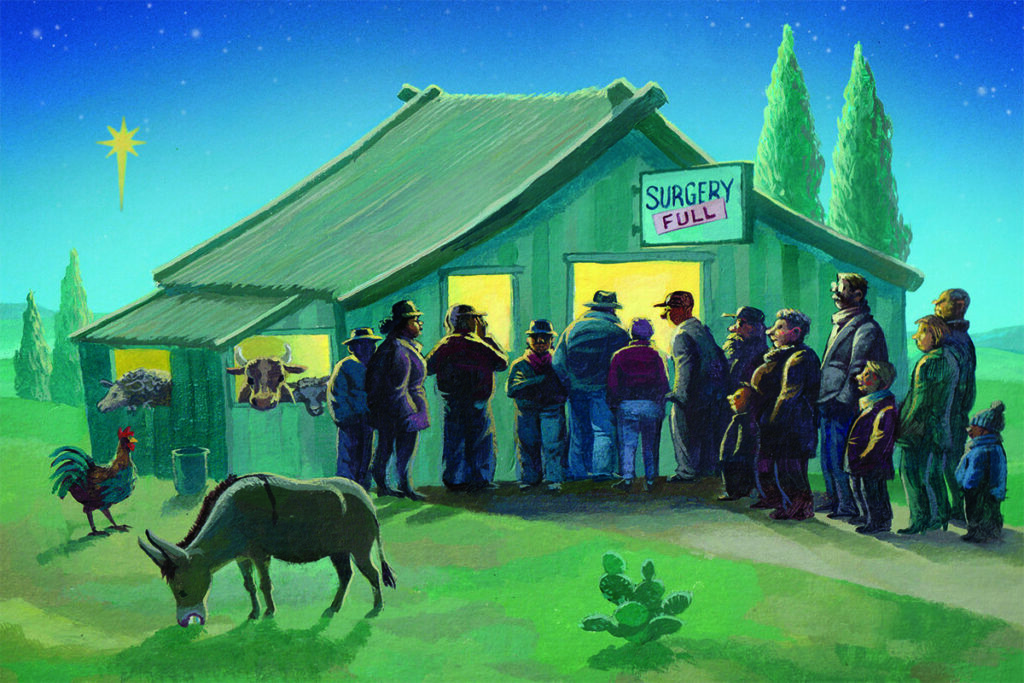

This year, the nativity story has unwelcome resonance for growing numbers of GPs, who are closing their lists to new patients in order to cope with demand. As part of a series on list closures, Eliza Parr investigates the implications for practices – good and bad
Increasing numbers of struggling practices are reaching for their final throw of the dice before handing their contracts back: closing their list to new mothers, fathers, holy infants and all those in between.
This is a significant step for GP partners, especially amid widespread patient concerns around access and the financial costs of closing a list. But for some practices, it can seem like the only way to rein in ever-growing workload while safely serving their current patients.
GPs have a formal and an informal route to close their lists (see box, below), which have both been promoted in recent years as ways of managing workload in a time of crisis. In response to the Government’s GP access plan in 2021, the BMA advised practices to apply to formally close their lists to prioritise core work. In Northern Ireland, where 7% of all practices requested list closure in 2022, the BMA GP Committee (GPC) last month published a ‘safe working’ guide for GPs, with formal list closure suggested as a method of controlling workload. Many LMCs offer similar advice.
The number of practices across the UK requesting formal list closure in 2022 was the highest in the five years that freedom of information (FOI) data have been available. Meanwhile, the rate of applications being accepted by ICBs and health boards was at its lowest, with only three-quarters of requests granted last year.
How to close a practice list
Formal closure
Under the GMS contract, practices can write to their ICB or health board, listing the reasons why a closure is necessary and any steps already taken to alleviate unmanageable workload. The two parties must then discuss if there’s another solution, perhaps involving the LMC, before the ICB makes a decision within 21 days of receiving the application. If accepted, the practice must close its list for at least three months but no more than 12 months.
While this route requires more bureaucracy, a formal list closure does mean the commissioner won’t continue to assign patients to the practice. However, practices must continue to allow registration by immediate family members of their current patients.
Informal closure
According to BMA guidance, practices can take ‘informal list measures’, which essentially means declining to register any new patients but without having to get permission from their commissioner. The BMA says this is still within the independent contractor’s rights. Under the GMS contract, practices have the right to refuse applications for inclusion in the list of patients if they have ‘reasonable grounds’. These grounds do not explicitly include workload pressures or concerns about safe working, however the BMA says it would not consider taking these measures to be a breach of contract. The union says it is not aware of a remedial notice ever having been issued for this reason.
If refusing a patient application, practices cannot discriminate based on age, appearance, disability or medical condition, pregnancy or maternity, race, religion or belief, sexual orientation or social class.
If practices take this ‘informal’ route, they must inform patients who apply of the reasons for refusal. These list measures also do not stop the NHS board from assigning patients to the list. And although permission from commissioners is not necessary, the BMA says practices should initially consult them, and raise the matter with the patient participation group (PPG).
Pelaw Medical Practice in Gateshead, Tyne & Wear, got the green light from its integrated care board (ICB) to close its patient list in July this year, after one partner retired while another partner and the practice manager had taken sickness leave within six months. This coincided with an influx of patients because newly built local homes became available and a nearby singlehanded practice closed its doors.
Dr Ruth Aynsley, one of the two partners who remained, says: ‘We told the ICB we’re really struggling and that the practice manager leaving was the final straw. We wanted to talk about options, including handing the contract back or closing the list. The ICB explained the process to close the list and was really helpful. The application was quite cumbersome.
‘I think we’re doing better because of it – with people moving away from our list, we’ve probably shrunk by about 200 patients. We’ve got more stability. Psychologically, for me and the other partner who is left, it’s really helped to know we’ve got some control over what’s happening.’
Despite the breathing space a list closure allows, the obvious downside for practices is the loss of income. There is, of course, a reduction in global sum payments when a list becomes smaller (as patients move away or die without being replaced). Commissioners may also decide that practices cannot continue local enhanced services while their lists are closed.
Commissioners are under no obligation to grant list closure applications. In Northern Ireland, only four of 22 applications were granted last year. Northern Ireland GPC chair Dr Alan Stout says the criteria for application success are unclear and that commissioners’ refusals seem to be ‘overriding very significant patient safety concerns’.
That said, the Northern Ireland government last year set a temporary freeze on registrations to support patients during the winter. A spokesperson told Pulse: ‘In acknowledgement of the pressures experienced by practices over the winter period, the Department of Health had put in place a temporary patient registration freeze for all practices from 1 November 2022 to 31 March 2023. This meant that any patient who [was] currently registered with a GP practice in a locality area could not move to another practice within the same catchment area.’
Last year in Glasgow, 19 practices requested list closure, which is more than double the totals in previous years. However, unlike Northern Ireland, all of these applications were granted by the health board.
Dr Sheena Fraser, a GP partner at Waverley Park Medical Practice in Glasgow, says that last year her practice was running with around 500 patients more than they felt was safe. ‘We got to the end of our tether. So we said “enough, something is going to have to stop – if we don’t take charge now, we’re going to sink and continue to sink”.’ Dr Fraser got permission from the board to close the practice list in January 2023 for 12 months, and she says it has been a ‘reprieve’, reducing workload by around 18% and patient numbers by around 400.
But if closing the list fails to ease pressure, a practice may close its doors altogether. The number of practice closures has decreased from a peak of 163 in 2018, but remains high at 57 last year – which continues to have a domino effect on neighbouring practices.
Informal list closures
For practices that don’t want to – or aren’t allowed to – take the route of formal list closure, there is the option of informal list closure (see box, above). LMCs have promoted the idea too – earlier this year Leicester, Leicestershire and Rutland (LLR) LMC advised its practices that they can informally close their lists if they feel unable to provide a safe service.
In Suffolk and North East Essex ICB area, while only three practices applied – unsuccessfully – to formally close their lists over the period 2018-2022, there were 15 informal list closures. Also, this year 5% of the 400 GP partners responding to a Pulse survey said they had informally closed their lists, with a further 11% saying they were considering suspending registrations.
A GP partner at a practice in South East England took an informal route by alerting its ICB that the list was open to allocations only. The GP partner, who wishes to remain anonymous, said they ‘informally closed the list as there has been absolutely no support from the ICB or NHS England for the new housing without accompanying resources’. The GP said general practice is facing ‘increasing relentless demand’ and that closure was a ‘last resort’.
Another practice in Merseyside informally closed its list because of the impact of a neighbouring practice’s access and staffing issues. Patients left and started looking elsewhere, putting other practices under pressure. One GP partner said patients were approaching them ‘in large numbers that we couldn’t absorb’. This led to a ‘co-ordinated’ informal closure across three local practices, whereby patients who already had a GP in the area were not accepted. Commissioners were aware of this action, and supported the temporary measure to help practices stay afloat. But the GP partner says there should be a mechanism to agree a specific number of new registrations per month, because the practices have had to open and close their lists multiple times throughout the year to manage the flow.
For others, list closure is a call for help. In Oxfordshire, two neighbouring practices closed their lists in quick succession. A third closed its list informally. A partner at the third practice told Pulse it was a signal ‘that we do not have unlimited capacity’.
Only feasible option
It’s no secret that many practices are facing insurmountable pressures. With demand rising, the workforce declining and insufficient funding, practices are taking their own measures to avoid shutting down completely.
No GP partner wants to refuse new patients. But it may become the only feasible option for practices that are struggling to stay afloat.
This piece will appear in the December print issue of Pulse. We will have more on list closures and their effect all of next week
Additional reporting: Madeline Sherratt
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [3]
Please note, only GPs are permitted to add comments to articles











Simultaneously alarming and unsurprising. Imagine being asked to engage in unsafe practices, knowing that patient harm is likely to ensue. You’d be failing in your duty if did anything but decline. And yet just by allowing more patients to register, GPs are being sucked into doing just that. As ever, damned if you do and damned if you don’t. A familiar Catch-22.
Luckily, I’ve left GP having begun to dig my own tunnel out 30 years ago – after seeing the future trajectory written depressingly clearly on the wall. But I feel desperately sorry for those still struggling away and highly nervous as I tip-toe through my sixties just hoping for the best. I’m registered with an amalgamated practice and have sampled the delights of “working at scale”, aka impersonal, unresponsive and impenetrable practice. So too my family and friends, who regularly message or call me with “So sorry to bother you but I just can’t get to a GP….”
Would a change of government fix it? Well it didn’t last time. We just had bizarre imposed targets like the 48 hour wait initiative. That didn’t fix much.
No Christmas cheer here I’m afraid. It’s all pretty gloomy.
Best plan is to construct your own health record, use private online GP services for perfunctory care and stash some money away in Premium Bonds for pay-as-you-go interventions at the local private hospital as required. Rely on the good old NHS for life-threatening care only.
Really sad when you consider the days when we couldn’t get some GPs to retire. Now we can’t get them to stay…
Here’s a crazy idea…..why don’t ICBs/NHSE start offering/promoting new GMS contracts again?
Previously despised by those in power, GMS contracts were replaced by PMS/APMS, in an attempt to destroy the perceived lazy limpet-like Partner power-base.
But to their horror, it turns out the old GMS system gave security, continuity, stability, high quality and value for money compared to the cowboy capitalists squeezing APMS for every penny whilst providing abysmal care and swanning off as soon as the money dried up, leading to closures and chaos.
If we now have full surgeries with no room at the inn, but with “doctors on the dole” (pushed out by ARRS) kicking around looking for work, why not bring the wheel full circle and encourage these superfluous GPs to set up their own GMS partnerships in under-doctored areas?
Back To The Future, anyone??
Or we could change what is ‘basically a sickness service, to a neighbourhood health service’ and call it a WES?
SIMPLES