
Pulse’s newest investigation revealed new data on the number of practices applying to close their patient list – a last throw of the dice before handing back their contract. As part of this series, Eliza Parr explores why practices might take the formal route and what impact it has
Practices who have taken the step to formally close their patient list will know it is no easy task. Getting permission from local commissioners can be a laborious process, taking up valuable time when a practice is likely already under huge pressure.
So it’s no surprise that many GP partners describe it as a ‘last resort’ – an attempt to keep the practice afloat and avoid handing back the contract.
While certainly not a cure-all, some practices have had success with a formal list closure as it allows them the breathing space to do some forward planning, rather than constant fire-fighting.
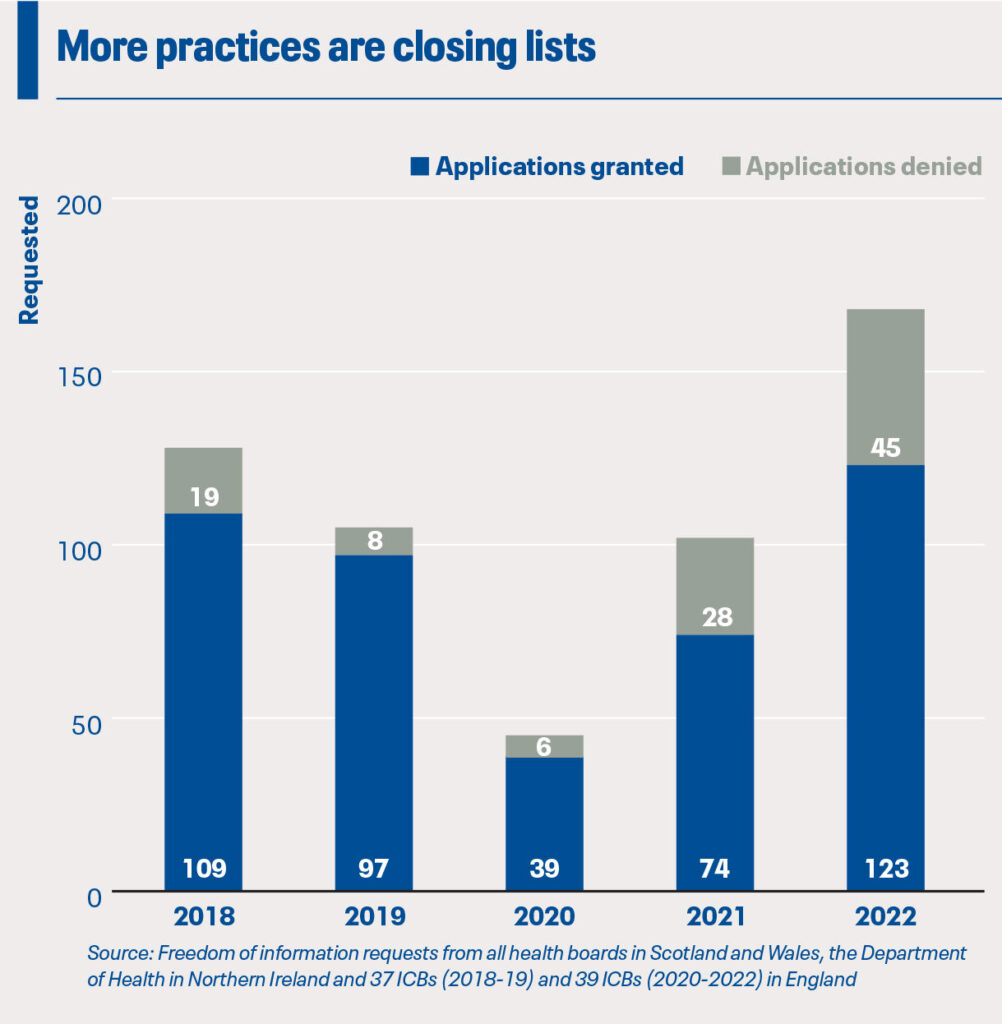
Nevertheless, the rising number of practices reaching for this last resort is worrying – last year, the number of practices across the UK requesting formal list closure was the highest it’s been in the five years that freedom of information (FOI) data have been available.
And although formal list closure has been promoted in recent years as a way of reining in workload, more needs to be done to address the underlying issues which lead practices to breaking point.
How does it work?
Formally closing the practice list is allowed via the GMS contract, but it isn’t always a simple process.
GP partners must write to their ICB or health board, listing the reasons why a closure is necessary and giving evidence they have tried other routes to ‘alleviate difficulties’. The contract also says practices must include details of any discussions with their patients, showing their ‘opinion’ on whether the list should be closed.
Practices should also state the proposed time period over which they want to keep the list closed – it must be at least three months but no more than a year.
Local commissioners and the GP practice then discuss if there’s another solution, potentially involving the LMC, before the board makes a final decision within three weeks of receiving the application. If accepted, practices can’t submit another formal list closure application until after a period of 12 months.
If rejected – which is becoming increasingly common – the ICB or health board must give its rationale to both the GP practice and the LMC. Another application can be made after three months.
This route requires more bureaucracy than an informal closure. Dr Ruth Aynsley, a GP partner in Gateshead who closed her practice’s list earlier this year, says the application is ‘quite cumbersome’, with each step taking a couple of weeks. ‘Of course, there’s no time to do that in the day, so you’re spending the evenings trying to do those things,’ she adds.
But a formal list closure does mean the commissioner won’t continue to assign patients to the practice, although practices must still allow registration by immediate family members of their current patients.
The picture across the UK
While the number of list closure applications is the highest it’s been in five years, the rate of applications being accepted by ICBs and health boards was at its lowest. A quarter of applications were rejected last year, and the issue was most acute in Northern Ireland where out of 22 applications, only four were granted.
GPC NI chair Dr Alan Stout says the Department of Health does not give ‘any particular rationale’ when rejecting applications. ‘There seems to be some criteria, which I don’t know what they are, that are overriding very significant patient safety concerns. And I don’t think that’s right, I don’t think it’s a position that we can stand over.’
Over the past year, general practice in Northern Ireland has been in crisis – 19 practices have handed back their contract since July last year, and during that time the country has been without a first or deputy first ministers. Dr Stout says the demand on GPs is ‘crazy’ and ‘unmanageable’, so for some practices, formal list closure may be the only way to stave off a contract handback. In fact, the BMA NI advised GP partners to consider formal list closure in their recent ‘safe working’ guidance.
But many practices will have to use other methods of managing workload if the acceptance rate for list closure applications remains so low (at 18%). In Derry, GP partner and BMA NI chair Dr Tom Black applied earlier this year due to unmanageable workload, but after a long waiting period the Department of Health rejected the request.
Dr Black says: ‘There are other practices in Northern Ireland who have applied for list closure and been declined. My concern is that the only practices who seem to be allowed to have a list of closure are those practices which have already handed back their contracts. Now, that seems to me an extraordinary state of affairs.’
Although GP leaders continue to have concerns, the Northern Ireland Government did take some action last year. To help struggling practices, they set a temporary freeze on registrations for patients who already had a GP in the area to support practices during the winter. However this only lasted from November 2022 to the end of March 2023.
Scotland is also seeing a high number of formal list closure applications – but with an acceptance rate of 100%. Last year, this accounted for just under a third (53) of the total applications across the four nations. Glasgow LMC medical director and GPC Scotland deputy chair Dr Patricia Moultrie says the number in Glasgow (19) is a significant increase on previous years, when they’d expect to only have one or two practices closing their list.
This points to a ‘significant gap between capacity and demand’, including the usual recruitment problems, according to Dr Moultrie. The high number of closures has been ‘fairly stubborn for some time now’, and as of October 2023, 20 out of the 227 practices in the Glasgow area have closed lists.
Dr Moultrie adds: ‘We feel there’s a number of things coming together. I mean, obviously practices are struggling to recruit. We know that the long hospital waiting lists cause increased work in general practices.
‘Our sense is that patient health seeking behaviour has changed over the course of the pandemic too, possibly partly because of mental health problems and cost of living crisis.’
Impact of a formal list closure
When a practice closes its list, there is an inevitable impact on neighbouring practices who might experience an increase in patient registration requests. Dr Amir Hannan, chair of Greater Manchester LMCs, says the situation for practices with closed lists in his area has been ‘very, very uncomfortable not just for them but for the surrounding practices’.
Similarly, Gateshead and South Tyneside LMC chair Dr Paul Evans says his own practice has been affected by a local list closure. ‘It has certainly put pressure on [the practice’s] neighbours. Obviously, their neighbouring practices are already under pressure, because of the fact that another practice had closed earlier this year and all the practices in the area have taken patients from this practice.’
And Dr Moultrie says that it is a ‘very much a last resort’ for practices because they are ‘very conscious’ of the impact on their colleagues in nearby practices.
Given this potential domino effect, making a formal list closure application is certainly not a decision that is taken ‘lightly’, according to Leicester, Leicestershire and Rutland LMC chair Dr Grant Ingrams. He says the main reasons practices take this measure are recruitment issues or lack physical space. ‘The process is stressful enough – no practice in their right mind is going to put themselves through that stress unless they’ve got a significant problem.’
Staffing was a key issue for the GP partners at Pelaw Medical Practice in Gateshead. Within six months one partner retired, while another partner as well as the practice manager went on sickness leave. Dr Aynsley, one of the two remaining partners, tells Pulse that getting permission from the ICB to close their list for six months has given them a ‘bit of breathing space’ and stopped the size of their patient becoming unmanageable.
So a formal list closure can help turn a crisis around for practices. But they should be mindful that the ICBs and health boards are increasingly exercising their right to reject applications.
And even after getting a green light, there is an inevitable loss of income. As patients move away or die without being replaced, the total list size reduces resulting in lower global sum payments. At a time when practices are already struggling with financial viability due to the cost of living, staff pay uplifts, and stagnant core funding, this reduced income could be crucial.
Formal list closure is not yet commonplace – while the number of formal applications has risen over recent years, it remains only a small proportion of the total number of UK GP practices. However, this could be the early signs of a rising trend.
Pulse’s survey of over 400 GP partners earlier this year found that 3% of practices had formally closed their list in the past year. Importantly, however, 11% had not closed but were considering it.
As practices run out of survival tactics amid cost and workforce pressures, more patients may find themselves being told there is no room at the practice.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













In old days it was a figure of 3500 patient for single handed as maximum number of patients and no more payment if it goes over. No more assignment of patients after this number achieved.