Key points
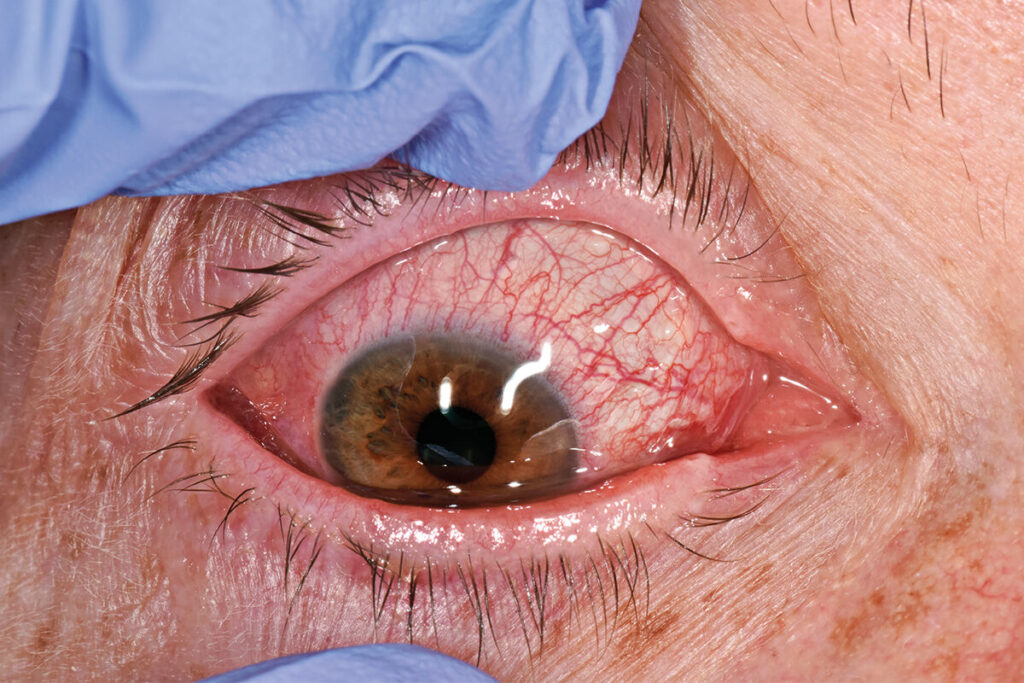
- Red flags for serious eye conditions requiring urgent referral are: visual loss; pain; photophobia; history of contact lens wear; temporal arteritis symptoms; and post-operative pain and redness
- Management of viral and bacterial conjunctivitis is essentially the same, except that bacterial conjunctivitis may require topical antibiotics or urgent referral if there is copious discharge
- Acute (closed angle) glaucoma typically presents with unilateral visual loss, pain and congestion of the cornea; these may be preceded by episodes of ‘halo’ vision or blurring and there may be a reduced pupillary light reaction on the affected side
- Around 15% of herpes zoster cases result in herpes zoster ophthalmicus (HZO) or ‘facial shingles’ which should be referred urgently if the eye is red or painful, or there is visual loss; rashes affecting the tip of the nose are associated with a high risk of complications (Hutchinson’s sign).
- Herpes simplex is one of the commonest causes of central corneal infections; fluorescein staining may reveal the ulcer and vesicular lesions may be present on the eyelid. Suspected cases should be referred for urgent slit-lamp assessment.
- Suspected neonatal conjunctivitis – occurring five to 19 days from birth and causing mucopurulent discharge and red conjunctiva – is a medical emergency, and a notifiable disease.
Dr Anup Shah is a GP and GPSI with Moorfields Eye Hospital NHS Foundation Trust, London, a member of the Royal College of Ophthalmology and a lecturer for Primary Care Ophthalmology
Q: Specialists use slit lamps when diagnosing red eyes but few non-specialists have the skill and even fewer have the kit. What examination can we carry out with the basic equipment we have?
Once you have taken the history, the most important part of an examination is a corrected Snellen visual acuity test in each eye. Test each eye individually, with distance glasses if the patient needs them. If they don’t use glasses, you can measure their vision through a pin-hole, which will eliminate any refractive error. If they have any visual loss on testing, it is important to know why.
The rest of the examination will depend on their history. Look at the front of each eye: at the cornea, conjunctiva and iris with the naked eye, checking for any abnormality compared with the other side. Then stain with fluorescein (instilled into the lower lid) and look at the cornea with a blue light filter. Green fluorescence will reveal corneal lesions. Then evert the upper eyelid, to look for foreign bodies if suspicion is raised by the history.
Next, use the ophthalmoscope to check the red reflex to see whether the lens is clear or there is a cataract or other obstruction. Use a bright light to test the pupillary light reflex and check for a relative afferent pupillary defect. Use the ophthalmoscope to look at the optic disc and macula. Note that visualising retinal structures through an undilated pupil can require practice.
Click here to read the full article and download your certificate logging 2 CPD hours towards revalidation
Not a Pulse Learning member? Click here to join and gain access to over 400 CPD modules
















