GPs should downgrade some urgent colorectal cancer referrals based on new FIT threshold
GPs should downgrade some urgent colorectal cancer referrals based on new FIT thresholds, new guidance has recommended.
Patients with a FIT test result below fHb 10μg Hb/g should not be referred via the urgent cancer pathway even if their symptoms fulfil NICE criteria, it said.
NHS England said in January that GPs must conduct FIT tests for all ‘urgent’ referrals for suspected lower GI cancer.
But the new joint guideline from the Association of Coloproctology of Great Britain & Ireland (ACPGBI) and the British Society of Gastroenterology (BSG) has now said that GPs should conduct the tests in order to establish whether patients require an urgent referral in the first place.
It said: ‘We recommend that FIT should be used by primary care clinicians to prioritise patients with clinical features of colorectal cancer for referral for urgent investigation.
‘FIT is a triage tool to identify those patients with symptoms of suspected colorectal cancer who should undergo further colorectal investigation.’
The guideline, initially published in summary form and welcomed by NHS England, recommended that a ‘FIT threshold of fHb ≥10μg Hb/g should be used in primary care to select patients with lower gastrointestinal symptoms for an urgent referral pathway for colorectal cancer investigation’.
However, it added that patients ‘should not be excluded from referral from primary care for symptoms on the basis of FIT testing alone’ – suggesting that if their FIT result is below fHb 10μg Hb/g, they should be downgraded to a routine referral.
And it said that ‘some patients with symptoms of suspected colorectal cancer may be managed in primary care if fHb <10μg Hb/g’, as long as ‘appropriate safety netting is in place’ and the GP does not have ‘ongoing clinical concern’ about any ‘persistent and unexplained symptoms’.
This contradicts current NICE guidance, which recommends various scenarios where patients should have an urgent referral for suspected colorectal cancer, without the need for a FIT test.
However, a spokesperson for the BSG told Pulse that overall they expect more people will be referred as a result of the guideline.
They said: ‘The guideline does not state that GPs should not refer patients with symptoms. The use of a FIT test is vastly superior to relying on symptoms alone in the identification of people who are most at risk of bowel cancer, as it is a much more sensitive method.
‘People with what were previously considered “high risk symptoms” can still be urgently referred but the approach is tailored and nuanced according to patient need.’
They added: ‘In fact, evidence indicates that a high-risk symptom is a symptom with a raised FIT concentration.
‘Therefore, those with what are currently considered “low-risk symptoms” are more likely to be diagnosed, as are those who are younger e.g. below 50, who present to their GP with symptoms.’
The guidance also recommends:
- GPs should ‘follow up patients with no FIT result to encourage them to return a sample or, where the kit has been lost or inadequately submitted, offer a further test’
- Patients who ‘decline to return’ a FIT test should be ‘counselled that evaluation of their symptoms is incomplete’ and ‘encouraged to complete their test’
- Services should ‘consider ways of promoting a high proportion of patients to return FIT kits’
- GPs should use ‘existing national and local guidelines’ to assess the risk of colorectal cancer if ‘no FIT result can be obtained’
- FIT could be utilised for patients with iron deficiency anaemia within primary care to inform urgency of referral
- It could also be used to ‘stratify’ adult patients aged younger than 50 years with bowel symptoms suspicious of a diagnosis of colorectal cancer
- Patients with persistent or recurrent anorectal bleeding should be referred for flexible sigmoidoscopy if fHb <10μg Hb/g
- There is ‘currently insufficient evidence to recommend including FIT in a risk score with other clinical features to identify patients with symptoms of suspected colorectal cancer’
The new guidance concluded: ‘On the basis of limited evidence, clinicians and patients consider FIT as an acceptable test for symptomatic colorectal cancer in most circumstances.
‘We recommend that FIT, as a diagnostic triage tool, can be implemented safely at primary care level, and that a programme of education be developed to facilitate implementation of FIT in primary care.’
It added that the guideline will be published in full ‘shortly’ after being presented at the annual BSG conference in Birmingham this week.
An NHS England spokesperson told Pulse on background that although it did not commission the guidance, it is recommending GPs utilise it to help identify cancers earlier.
NHS England primary care medical director Dr Nikki Kanani said: ‘FIT kits are an extremely valuable tool we already use in screening for bowel cancer – they are far easier for patients to use – so we welcome today’s guidance recommending GP team to use these tests to help diagnose people presenting with signs or symptoms sooner.
‘Detecting cancers as early as possible gives people a much better chance of beating the disease when it is easier to treat and the rollout of these kits across primary care will certainly help in our drive to catch cancers earlier and ultimately save more lives.’
The spokesperson added that the adoption of more FIT kits in primary care will free up capacity for clinicians to prioritise colonoscopies for those who need it most and that a new data collection monitoring FIT kit use across primary care will be available from July.
Hertfordshire GP partner Dr Kevin Barrett, who is part of the Primary Care Society for Gastroenterology (PCSG) committee, told Pulse: ‘A FIT test can be useful to help secondary care prioritise patients who need urgent investigation and therefore help those at highest risk be investigated, diagnosed and treated sooner.
‘However, we have to be allowed to trust our gut instincts and there should always be a way to allow clinician:clinician communication so that those patients we are worried about do not miss out on timely care if they don’t meet a particular set of referral criteria.’
Chief executive of Bowel Cancer UK Genevieve Edwards said the charity is ‘hugely excited’ by the ‘transformational’ guidance but warned that GPs ‘will need support to put the guidance into practice’.
She said: ‘Almost 43,000 people are diagnosed with [bowel cancer] in the UK every year and those with low-risk symptoms – particularly those under 50 – often have to see their GP a number of times before being referred for further tests, which can lead to a delay in diagnosis.
‘This new guidance will help GPs to better identify and refer the right patients more quickly, and to help rule out bowel cancer first, not last. GPs will need support to put the guidance into practice and we look forward to working with the clinical community to ensure this is done consistently throughout the country.’
Alongside the new guidance, GPs working in primary care networks (PCNs) are being incentivised to increase FIT testing in one of three new Investment and Impact Fund (IIF) indicators introduced in 2022/23, backed by £5m in funding.
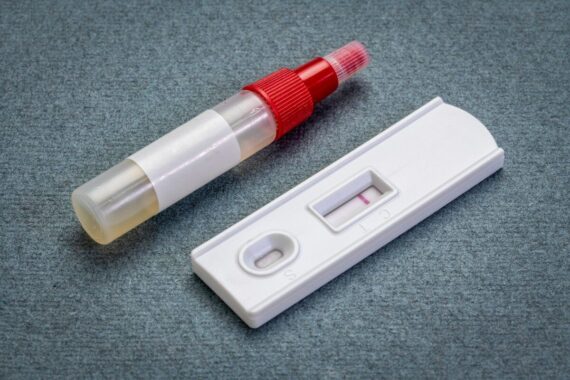
FIT tests are also used as a primary test in England’s national NHS bowel cancer screening programme, with those eligible sent a home kit every two years.
NICE guidance on GP referrals for colorectal cancer
Refer adults using a suspected cancer pathway referral (for an appointment within 2 weeks) for colorectal cancer if:
- they are aged 40 and over with unexplained weight loss and abdominal pain or
- they are aged 50 and over with unexplained rectal bleeding or
- they are aged 60 and over with:
- iron‑deficiency anaemia or
- changes in their bowel habit, or
- tests show occult blood in their faeces. [2015]
Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for colorectal cancer in adults with a rectal or abdominal mass. [2015]
Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for colorectal cancer in adults aged under 50 with rectal bleeding and any of the following unexplained symptoms or findings:
- abdominal pain
- change in bowel habit
- weight loss
- iron‑deficiency anaemia. [2015]
Offer testing with quantitative faecal immunochemical tests (see the NICE diagnostics guidance on quantitative faecal immunochemical tests to guide referral for colorectal cancer in primary care) to assess for colorectal cancer in adults without rectal bleeding who:
- are aged 50 and over with unexplained:
- abdominal pain or
- weight loss, or
- are aged under 60 with:
- changes in their bowel habit or
- iron-deficiency anaemia, or
- are aged 60 and over and have anaemia even in the absence of iron deficiency. [2021]
Source: NICE
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.
Related Articles
READERS' COMMENTS [8]
Please note, only GPs are permitted to add comments to articles












Nope
NG12 symptoms = 2WW with a FIT request at same time (if appropriate) for me. Secondary care cc’d into result and stratify as appropriate.
Seem to recall DES isn’t ALL it’s 40% or 80%
Have plenty of evidence locally never got above 30% attached to 2WW in our CCG and cancers found in FIT -ve
I also assume plenty of Primary Care Clinicians attended this meeting??
Fairly certain secondary care can decide how to investigate a patient with worrying symptoms just as much as primary care.
In next year’s guidance 2ww referrals will only be accepted for those who have had a community colonoscopy showing a lesion they can biopsy.
And in 2024 it will only allow a 2ww referral if that biopsy has come back showing a malignancy.
The common sense question is , what are GPs expected or liable to do if you have a borderline reading , say 9ug Hb/g and symptoms (other than rectal bleeding and sign of anorectal or abdominal mass) are present?
Are GPs liable to repeat FIT after an well agreed time interval ?
Surely , BSG is trying to manage the workload gastro services are facing right now but NICE also had its say
USUAL STORY OF NHS ENGLAND AND GUIDANCE ATTEMPTING TO “SHIT” ON GPs (apologies for pun). WE ARE ALWAYS EXPECTED TO HOLD RISK WHILE SECONDARY CARE ARE EXPECTED TO HOLD NO RISK…..WELL F*** O**…..WE ARE NOT HOLDING RISK, NO, SORRY BUT SWIVEL……NO, I SAID, NO, IT WON’T HAPPEN……….
But haven’t ‘They’ just decided that suspected cancer referrals can be organised by having a quick nip-in to the nearest Boots and a chat with the pharmacist?
Until NICE guidance changes (suspected cancer guidelines and FIT guidance). Medico-legal advice said that GPs could be liable for any delays in diagnosis.
If the society representing the coloproctologists want to downgrade referrals, do it by lobbying NICE and sending out the FIT tests themselves so they get the results directly.
Why does NHSE put the clinical risk on GPs? the GI team can send them themselves.
Once NICE have altered both guidances, then ask GPs to do it…..
Erm.. no! NG12 symptoms -> 2WW with pending FIT.
I have no idea who is on the 2WW list waiting for a scope, which patients have FIT 10 or FIT 1000 etc. If secondary care want to risk stratify and sensibly prioritise referrals using the FIT result, based on their knowledge of their own waiting list and capacity, WHILE holding their referral, then THAT seems entirely reasonable. Anything else would be a stupid transfer AND increase of risk and work.
The Acute hospitals have the majority of the NHS budget. They can afford to manage these patients.
Do Gastroenterologists no longer want to see patients?
The Hospital can employ PAs or ANPs to see them instead.
The number of gastro consultants has increased significantly.
Are they trained just to be technicians, ‘scope jockeys’?
Happy in their endoscopy suites but clueless with actual patient care?
This is specialist work.
The same specialists complain that too many patients present as emergencies with colorectal cancer.
The same specialists are attending coroners courts and GMC hearings blaming GPs for not referring.
The BGS is making its recommendation on a risk level which is significantly different from that recommended by NICE.
Instead of generating this opposition they could be working with GPs to develop safe systems.
The key to these systems is not blanket and incorrect barriers to referral.
The current volume issue is important, but this is not the way to improve it.
The key is about understanding the needs of the patients and working to reduce the barriers.
The higher the barriers the more everyone fights to get over them.