Speak up
This site is intended for health professionals only
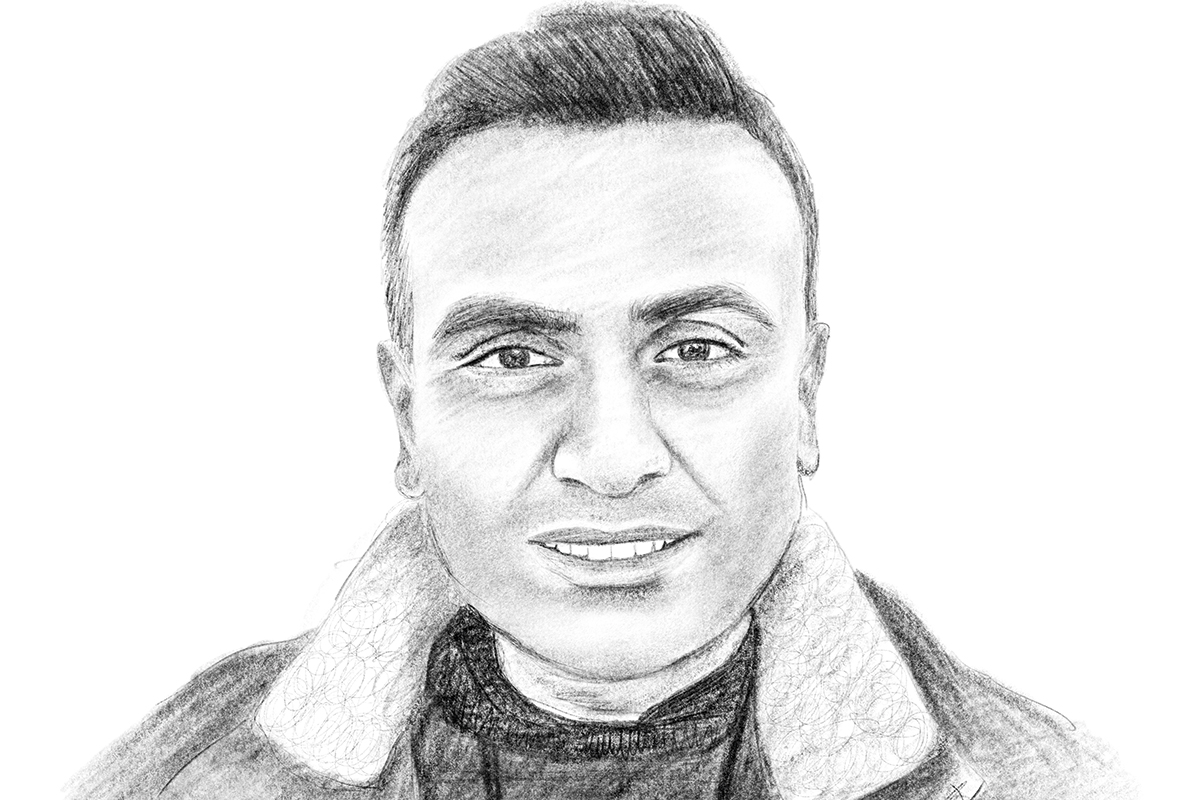
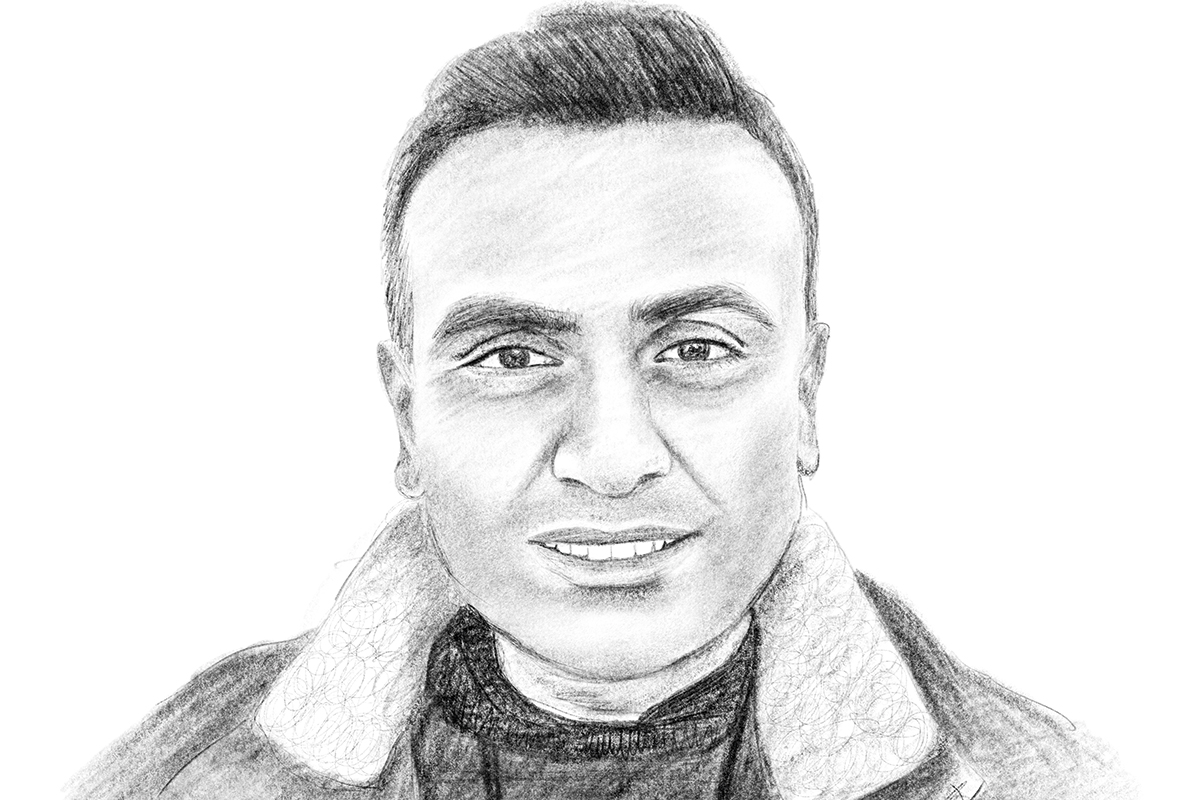
Primary care has to be listened to – and the current review of how PCNs will work within ICSs is a chance to be heard, says Dr Pramit Patel in Pulse PCN’s spring edition
With statutory integrated care boards on the horizon, primary care has an unrivalled opportunity to harness its local knowledge to deliver better services for patients.
While the pandemic has facilitated greater service collaboration, we all feel the NHS can still be disjointed and siloed in its approach. Now, we have the opportunity to build on the best of system working and to use the expertise of primary care with an independent national review, led by Professor Claire Fuller, who will look at how systems can drive more integrated primary care services at local level.
I work with Professor Fuller in our ICS, and I know she has a genuine drive to empower primary care to do better for our populations, and is committed to a true bottom-up approach.
The review will seek arrangements that are already working well in some areas of the country, and enable them to be developed nationally by developing guidance, infrastructure and removing obstacles.
Examples include South West London Primary Care Provider Alliance, which brought together primary care organisations to share learning, challenges, successes and priorities. That has evolved into a forward-looking partnership that rose to the challenge of winter pressures. It teamed up with out-of-hours urgent care providers to deliver additional capacity in the 111 service and additional practice call-handling linked to directly bookable face-to-face appointments in extended access hubs across south-west London.
In Sheffield, a team of GPs has had training and mentoring from hospital consultants, which enables them to guide primary care colleagues who think a patient needs to be referred to secondary care. Instead of making a referral the GP can be advised on how to treat, or whether to order further tests or supply further information. Sometimes, community-based services may be suggested as an alternative to a hospital outpatient appointment. This arrangement means patients are more likely to get the treatment they need without having to go to hospital, the quality of referrals improves and GPs gain enhanced knowledge.
The review aims to identify these kinds of local excellence, to assess how transferable they are and consider how ICS leaders can make them happen on their own patches. This can open the door to improvements and more collaboration across the whole system, particularly in primary care. The review is about far more than provider trusts talking to other provider trusts.
While there is no simple fix for the myriad of issues facing primary care, this can be a catalyst for improvements, whether that’s tackling bureaucracy, providing commissioning powers at place level, or funding better leadership development.
Primary care has to be listened to, and this review – which we are calling the Fuller Stocktake – is a clear opportunity to be heard. So let’s speak up.
Contact the NHS Confederations primary care team at PCNnetwork@nhsconfed.org or visit fullerstocktake.crowdicity.com
Dr Pramit Patel is chair of the NHS Confederation’s PCN network and GP clinical director for Care Collaborative PCN, Surrey Heartlands.

Register today to receive weekly newsletters and a free copy of Pulse PCN with Pulse magazine
Sign up now