Case 1
Mrs A, age 35, has just had a positive pregnancy test and visits her GP to discuss pregnancy. She also mentions that in the last few days she has been feeling generally unwell with non-specific symptoms and a mild upper respiratory tract infection. On examination she has a very fine maculopapular rash over her torso and extremities. The GP diagnoses mild viral illness. The patient remains well and is not seen again. The GP, however, sends booking bloods and the results are as follows:
- HIV Ag/Ab – negative.
- HBsAg – negative.
- Syphilis EIA – negative.
- Rubella IgG – positive.
The GP calls Mrs A with the results and reassures her. She has no further symptoms and has completely recovered, and is referred to the nearest maternity unit. She is abroad when due for the 20-week scan and re-arranges this for 28 weeks’ gestation. In this scan, severe asymmetric intrauterine growth restriction is diagnosed, and brain calcifications are noted. Amniotic fluid is tested for the presence of viruses and rubella RNA is detected by polymerase chain reaction. Retrospective testing of the booking sample reveals that rubella IgM and rubella IgG were detected – rubella IgG was of low avidity, indicating a recent infection. The woman had no history of MMR vaccination and was originally from a country where rubella is endemic. She had family visiting and one of the visitors had similar symptoms at the time.
GP’s diagnosis
Mild viral illness – rubella immune at booking.
Actual diagnosis
Rubella infection in the first trimester.
Clues
The history and documented examination of rash early in pregnancy. This should have been investigated properly at booking. Pathogens such as rubella, measles and parvovirus should be part of the differential diagnosis of maculopapular rashes in pregnancy, as well as HIV and syphilis. The latter should be tested regardless of booking blood results as women might acquire these infections in pregnancy.
Take-home message
Investigate all viral-type rashes in pregnancy. Take a careful history of vaccination and interpret the results with caution.
Case 2
Mr F is 23 and presents with a two-day history of aches and pains and an odd-looking rash all over his body. He just came back from Thailand, where he had a sore throat. He is on an antibiotic. The GP suggests the rash is probably an allergic reaction and recommends stopping the antibiotic. On examination the patient has a red throat with no exudate and a widespread palpable rash. He goes home and comes back a few days later with a fever, feeling worse, and with symptoms and signs of altered consciousness. The GP refers him to the local A&E where a lumbar puncture after a CT of the head is performed – 600 lymphocytes, mildly raised protein and lowered glucose were identified. A diagnostic serological test was performed and treatment was initiated.
GP’s diagnosis
Drug allergy.
Actual diagnosis
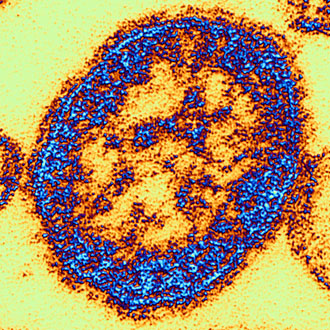
Primary HIV infection (PHI) with CNS involvement – a fourth-generation HIV antigen/antibody test was positive. At this stage, the laboratory was unable to type the infection as seroconversion-only antigen is detected and typing assays require presence of antibody. HIV-1 proviral DNA polymerase chain reaction was, however, positive – suggesting an HIV-1 infection. A repeat serological test a week later was requested as diagnosis of HIV infection requires two positive tests. Antibody was now present and typing confirmed HIV-1 infection.
Clues
The travel history, and a young man presenting with a rash and non-specific symptoms.
Take-home message
Take a sexual exposure history, as the above presentation can be compatible with HIV seroconversion or primary syphilis.
Case 3
Mrs K is 68 with a history of COPD. She is currently on prednisolone 40mg od for 14 days – this is the second course in the last three months. She presents with a history of feeling ‘under the weather’ and her husband reports some memory problems, claiming that she has not been ‘her usual self’ over the last couple of days. She has a normal neurological examination. The GP arranges a referral to a neurologist.
Unfortunately there is a delay in arranging the appointment in the neurology clinic and the patient deteriorates over the next couple of days. She presents at the local A&E with fever and altered consciousness. A lumbar puncture is performed after a head CT. There are a few lymphocytes in the cerebrospinal fluid, protein is raised and glucose is normal. There are 100 red cells, although this was not a traumatic tap. HSV1 is detected by polymerase chain reaction. Unfortunately, the patient develops permanent CNS sequelae following a stormy inpatient admission.
GP’s diagnosis
Early dementia.
Actual diagnosis
HSV encephalitis.
Clues
Altered behaviour, memory loss and prescription of steroids.
Take-home message
Patients on high dose steroids or immunosuppression might have atypical presentations. The high mortality and significant morbidity of this condition requires urgent lumbar puncture and initiation of intravenous aciclovir at 10mg/kg tds. Fever is present in 90% of cases and should be part of the examination.
Dr Eleni Nastouli is the lead consultant in virology at University College London Hospital