
Money – SUO
Austerity started for the NHS in 2010, but for GPs real-terms funding decreases have been a fact of life since the initial rise after the advent of the 2004 contract.
But after promises to ‘turn practices around’, it seems that NHS England may be putting its money where its mouth is, with the announcement that practices will receive a 3.3% funding uplift this year – the second year in a row they have seen an inflation-busting increase.
At the same time, practices will be freed from the bureaucratic nightmare of the unplanned admissions DES, have CQC fees reimbursed in full, and see improved reimbursement of sick leave payments.
For a profession that has been under the cosh for so long, this contract represents progress, if not a panacea. But there is still some doubt whether the uplift will bring the promised 1% pay increase and signal a move away from the austerity of recent years, which has seen a 13% fall in funding in the five years up to 2014/15 – the most recent official figures available.
Accountants warn this may be wishful thinking. They say much of the £239m uplift will get swallowed up by rising expenses, leading, at best, to an extension of the pay freeze.
For the first time in a long time it feels like they’ve got the message
Dr Krishna Kasaraneni
Michael Ogilvie, healthcare lead at OBC accountants, says: ‘I can find very little positive for doctors in the proposed contract. Yes, there is a 1.4% allowance for extra expenses – they will need this and more to meet cost increases.’
This is unlikely to come as a surprise to GPs who have seen it all before. Last year’s 3.2% uplift was supposed to lead to a 1% increase in pay. But a Pulse survey of 644 partners revealed that they suffered an average 4% pay decrease in the first six months of the financial year.
But GPC deputy chair Dr Richard Vautrey is keen to stress that ‘an average 1% pay uplift is something we should expect to happen’ this time.
He adds that the most recent official figures on pay, from 2014/15, showed partners and principals were able to give themselves a 1.7% pay increase that year – despite a ‘derisory’ 0.28% funding uplift.
A Pulse analysis of the contract agreement shows there will be around £11,000 for an average 7,000-patient practice to cover pay uplifts and increases in expenses – which includes staff costs, the general running of practice, accountancy fees and bank charges. This specifically excludes CQC and rises in indemnity fees, which are covered elsewhere.
But this is only for the ‘average’ practice and the biggest losers are those that rely heavily on the Minimum Practice Income Guarantee (MPIG), which is in the fourth year of a seven-year phase out, with the money being redistributed through the global sum. The same is true for those who relied on seniority payments, which is in the third year of its six-year phase out, and those suffering from PMS funding reviews.
Others will gain from the agreement. The minority of practices that didn’t undertake the unplanned admissions DES will see a boost as the DES funding is reinvested in the global sum.
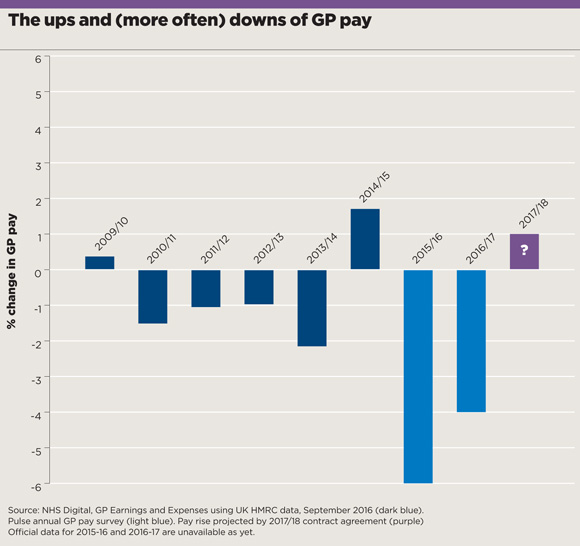
ups and downs of gp pay 580x546px March 2017 issue
But leading accountants warn the key factor determining a pay rise will be practices’ expenses – saying the 1.4% set aside allowed for this is insufficient.
Bob Senior, partner at RSM, points out inflation is likely to increase to 2.8% by 2018, saying: ‘I would have thought 2% would be more appropriate than 1.4%’.
Deborah Wood, healthcare services partner at Moore and Smalley and vice-chair of the Association of Independent Specialist Medical Accountants (AISMA), agrees there won’t be enough to cover 1% pay rises across the board. Reviewing official figures on expenses and likely inflationary costs, she concludes: ‘I think the situation is around a £5,000 shortfall in funding per practice.’
Of course, how badly practices are affected will partly depend on key areas of expense – predominantly their staff. Mr Ogilvie says: ‘Most practices find it hard to exist without paying for locums, and the increased cost of locums alone in some practices will eat up the extra allowance.’
Expenditure in other areas will also affect how much is left for pay rises. Individual practices will have CQC fees paid in full, but other pots of money, such as indemnity reimbursements, will be distributed using a flat rate, meaning practices that have suffered higher-than-average increases in fees will benefit less than those with smaller increases.
Related articles
No need for locum insurance cover, says GPC
Around 3% of over-65s will require new contractual frailty check, estimates GPC
GPC chair Dr Chaand Nagpaul says no contract can ever guarantee a pay rise as practices are independent businesses, adding: ‘We have put forward a package projected to enable a 1% pay uplift, but wider issues govern whether GP pay goes up or down, such as locally commissioned schemes and workforce expenses.’
NHS England chief executive Simon Stevens also acknowledged that the contract is ‘one piece of the jigsaw’, but added: ‘We’re now turning the corner on a decade of underinvestment in GP services, but with new cash clearly tied to new ways of working that both improve patient care and support family doctors.’
And while a pay rise through the national contract may remain wishful thinking for many, CCGs have been told by NHS England to provide £171m of ‘practice transformational support’ and the ‘sustainability and transformation plans’ – the local NHS blueprints – have been instructed to ‘increase investment in the out-of-hospital sector’. But with all areas of the NHS struggling, such resources are likely to entail new work for practices.
There is much to cheer in this contract – notably proof NHS England is starting to understand that GP workload is becoming unmanageable, and that any increase in workload should come with additional resources. It is notable that almost all the new responsibilities – such as checking overseas patients’ eligibility for free NHS treatment – have specific funding attached. Meanwhile, the end of the unplanned admissions DES frees up resources, with the replacement looking to be much less onerous.
As GPC education and training spokesperson Dr Krishna Kasaraneni puts it: ‘For the first time in a long time it feels like they’ve got the message.’
The bottom line may not change as much as GPs hoped, but, at the very least, life should get a bit easier for practices.
What an average practice can expect as part of the new GP contract?
£1,640 to cover the costs of the new work associated with the contract, such as checking the immigration status of new patients and the workforce census
£20,900 recycled from the unplanned admissions DES and put into the global sum to fund a new frailty checks scheme
This leaves around £11,500 to spend on pay uplifts and practice expenses, including staff costs, the general running of practice, accountancy fees and bank charges
The practice will also receive £4,526 to pay its CQC fees in full
And an extra £3,612 to cover the costs of increases in indemnity fees.
Other sweeteners agreed by the BMA and NHS England include:
- An extra £24 for every health check the practice does under the learning disabilities DES
- Increased sick pay cover, which will now be on a non-discretionary basis
- An increase in the value of a QOF point (undetermined as yet)
Source: Pulse analysis of figures stipulated in the 2017/18 GP contract agreement for England, based on an average practice of 7,000 patients receiving an extra £33,000 in their global sum payments (unweighted)

















