How normal service is being forced upon GPs
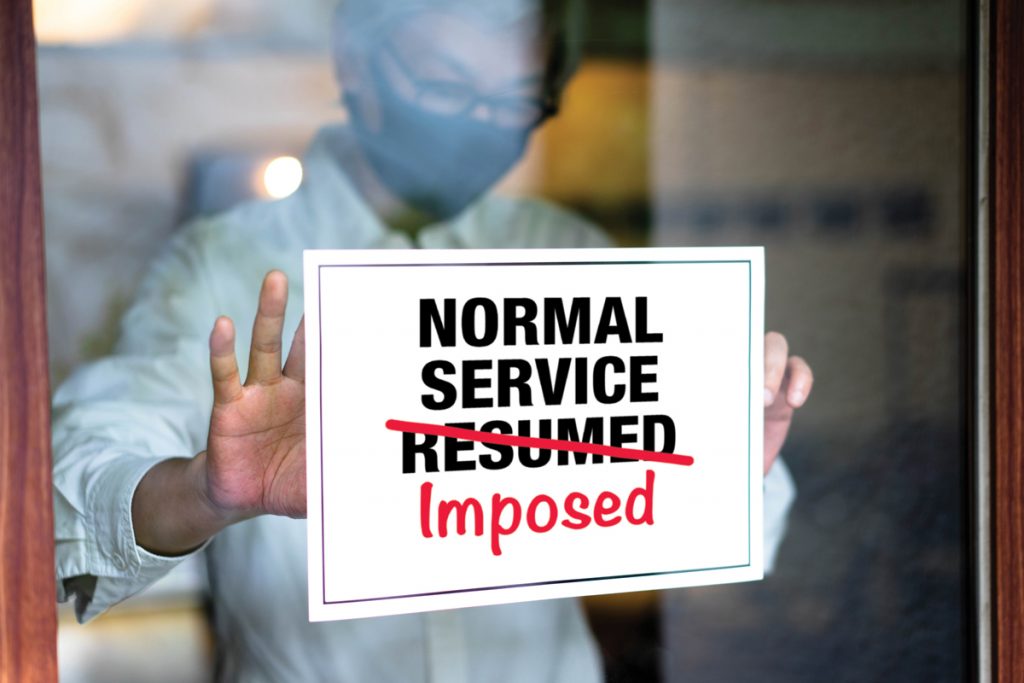
When NHS England instructed GPs to grant all patients face-to-face appointments when requested, it lost much of the profession’s goodwill. Costanza Pearce examines the fallout from the infamous letter
‘Practices should respect patient preferences for face-to-face care unless there are good clinical reasons to the contrary.’ So reads NHS England’s latest diktat to GPs.
The letter, sent on 13 May, tells practices they must also open their receptions to walk-ins within three days, with patients being triaged at reception.
In practice, this means any patient who requests an in-person appointment should be granted it, as long as they do not present a Covid-19 infection risk, NHS clarified.
The letter – which was incorporated almost wholesale into the Standard Operating Procedure on 20 May – caused a storm rarely seen in general practice. It was branded ‘tone deaf’ by the BMA and dismissed as a ‘memento to incompetence’ and ‘ridiculous’ by LMCs.
A petition calling for the resignation of NHS England medical director Dr Nikki Kanani has so far racked up 1,000 signatures.
The week after the letter, the BMA’s GP Committee agreed a motion expressing a vote of no confidence in NHS England’s executive team, and voted to cease all formal meetings with NHS England until the disagreement is resolved.
The ‘GPs are closed’ myth
The main reason for the anger is that the whole premise that GPs have ‘not been open’ is a myth. Where clinically appropriate, patients have been seen in person throughout the past year.
As Berkshire, Buckinghamshire and Oxfordshire LMCs put it in their statement: ‘Practices in our area have been working at levels which are not just at their full capacity but actually exceed their full capacity throughout the pandemic and more so over winter.’
The letter ignores the fact that many GPs have already returned to ‘business as usual’ of their own accord.
An exclusive Pulse survey of more than 800 GPs, held in the week leading up to the NHS England letter, found half were already doing home visits (54%) and non-urgent screenings (51%) as ‘normal’, with 35% saying the same for in-person enhanced services.
Furthermore, 9% said they were already offering face-to-face appointments as standard, while 25% said their reception was open.
Importantly, those who hadn’t yet moved to ‘business as usual’ had very good reasons for not doing so. It shouldn’t be forgotten that the main reason they began operating a ‘total triage’ model in March 2020 was because that was NHS England’s own guidance, implemented to reduce face-to-face care and minimise infection risk.
Despite this, NHS England has still seen fit to criticise GPs. Last September, it sent a letter ‘reminding’ GPs ‘that face-to-face appointments continue to be on offer, where clinically appropriate, in addition to video and phone consultations’.
The latest letter followed hostile coverage in parts of the media. It was released a few days after the Mail on Sunday launched a campaign continuing the narrative that practices have not been open, and calling for patients to be seen face to face ‘again’. The previous week, Telegraph columnist and repeat offender Allison Pearson claimed it was a ‘scandal’ that ‘you’ve not seen your GP recently’.
Practices aren’t ready
But alongside the anger, there is very real fear around the implications of the letter. More than two-thirds of GPs said they were concerned about their practice returning to ‘business as usual’ – a service comparable to that before the pandemic.
Around 70% of GPs cited low infection rates as ‘very important’ in the decision to open up services. With rising concerns over the India variant in the UK, it seems a perverse time to impose a blanket loosening of restrictions.
The BMA’s GP Committee chair Dr Richard Vautrey points out that social distancing is vital, but makes face-to-face appointments on demand impossible.
‘A surgery waiting room with space for 40 patients might now hold only six, affecting the number of patients who can be physically seen each day,’ he says.
Lincolnshire LMC medical secretary Dr Kieran Sharrock says the guidance leaves GPs in an impossible situation: ‘The expectation of the powers that be is that we’ll just go back to allowing patients to just book their appointments, but clearly we can’t do that. We need to socially distance and protect our patients and staff from infection.’
The sense of unfairness is exacerbated by the fact that NHS England is not applying the same rules to hospitals.
Hackney and City LMC chair Dr Vinay Patel said: ‘It’s not fair. In primary care, we are dealing with the consequences of hospital clinics not being at full function because they’re not seeing patients, so we are carrying a lot of the workload burden that may be generated as a result.
‘This message should have been allied across healthcare, not just focused on primary care.’
Workload
An even more pressing concern is the workload implications. GPs are already reporting being busier than ever and this guidance will exacerbate the problems, they warn, as patients have got used to digital access being freely available.
In Pulse’s survey, respondents scored ‘patient expectations’ highly as a factor influencing a return to normal services, with half saying this was an ‘important’ or ‘very important’ consideration.
As East Sussex GP partner Dr Chris Dixon puts it: ‘I am uncertain how we will cope with double the demand – people who like the new instant access against those who want face to face.’
The rise of e-consultation systems has increased workload. The UK LMCs conference earlier this month voted for a ‘full impact assessment’ of e-consultations amid reports of practices being ‘overwhelmed’ by demand.
NHS England’s letter adds open access to in-person appointments to the mix.
‘We’re seeing an increase in irritation from patients, who are expecting everything to be back to normal and have no idea about this tsunami of work which has landed on the health service,’ GPC deputy policy lead for education, training and workforce Dr Tim Morton tells Pulse. ‘We can’t continue safely at this rate.’
The days of clapping NHS staff are long gone, and patients now expect more than general practice can offer.
‘Those with minor issues still expect to be seen urgently’, says Surrey GP partner Dr Emma Watts, citing a patient who recently presented for ‘hair-ache’.
Enforcement
However, there is little clarity on whether GPs are obliged to act on the letter and Standard Operating Procedure. Many LMCs are advising they ‘have no contractual force’ and should be seen only as ‘guidance’. The BMA agrees: ‘It is for practices to determine how best to manage and deliver services and the best arrangements for appointments, based on expert knowledge of their community.’
NHS England emphasised the Standard Operating Procedure was a guideline.
However, Pulse later revealed CCGs had been contacting practices with a low proportion of face-to-face consultations, to ask how they planned to address this.
Contractual duty or not, GPs fear complaints if they don’t offer full online and face-to-face access: almost four in 10 respondents cited this as an ‘important’ factor in decisions to return to normal.
Future of digital provision
There are also potential long-term implications. This guidance seems at odds with the health secretary’s emphasis on digital provision. Matt Hancock, speaking in Parliament about the letter on 17 May, said the letter reiterated ‘the point that it is important to offer a face-to-face consultation for a patient who really wants one, while also using technology where that is the most clinically appropriate thing to do’.
How this is to be implemented going forward is anyone’s guess. Mr Hancock has long been a supporter of artificial intelligence triage, and it would not be a surprise if this is something he wants to see across general practice.
And maybe calls for ‘business as usual’ ignore the wider context – that ‘normal’ may well be different. Pulse’s survey showed a fifth of 836 UK GPs believe in-person appointments will never again be the default. Most tellingly, around 37% said they didn’t expect their waiting room ever to return to full capacity.
But come what may in the future, what GPs need now is for NHS leaders to show, once and for all, that they are on the profession’s side – rather than the media’s.
As Surrey and Sussex LMCs chief executive Dr Julius Parker says: ‘This latest letter panders to the illusion that the NHS can meet a limitless pool of patient demand… and throws general practice under the media bus.’
What is practices’ contractual duty?
The contractual requirements for practices are laid out in the GMS Regulations 2015, their subsequent amendments and any accessory legislation.
Practices are required to ‘have regard to’ all applicable guidance issued by relevant bodies, including NHS England. In other words, they should be aware of, consider and take into account guidance issued, but they are not contractually obliged to follow it. They may ignore it if they judge it to compromise other contractual, legal or ethical obligations.
The underpinning principle of the requirements of the regulations on practices is to meet the ‘reasonable needs’ of their patients ‘in the manner determined by the contractor’s practice in discussion with the patient’.
If any practice is uncertain about whether or not something they are being asked to do is contractually enforceable, they should always contact their LMC for advice.
Dr Matt Mayer is chief executive of Berkshire, Buckinghamshire and Oxfordshire LMCs
Related Articles
READERS' COMMENTS [12]
Please note, only GPs are permitted to add comments to articles













Talk about these horrible gps not giving everyone or anyone? F2F consultations! I can’ t even speak to my dentist’s receptionists to beg for an appointment in spite of losing 2 fillings and recently developing toothache.I get to leave a recorded message stating my case in order that someone can decide if it is safe enough to be in the same room as me.I did not even remember to tell them I have had my two vaccines( presumably like wot they have had! To date I have not had the courtesy of a reply.
Why are gps always portrayed as reluctant unhelpful players in the NHS.I left the BMA many years ago as I felt that as gp advocates they came no where near cutting the mustard.
I have recently retired but I can see the way general practice is going and it saddens my heart.
Just saying! But now I must re-fortify myself in the expectation of doing battle with the recorded message in my dentist’ surgery- wish me luck.
I had to F-F someone with an armpit “lump”.
I had to.
Purely, because of their “right” and obnoxious desire not to describe it on the phone.
In person, I said – point to it.
They grabbed the ENTIRE armpit fat and said what’s that?
I said it’s your fatty armpit.
I left it at that.
Cleaned the room.
And wasted 30 minutes.
SELF-ENTITLEMENT MADE IN BRITAIN/NHSE.
Interesting development and most definitely, sparking off serious debates .
In the beginning of this pandemic , I was looking for literature about the relationship between pandemics and human conflicts (war at the most serious level ) in history. I think ,almost invariably, pandemic is a call from nature to human beings that the ‘old’ ways could not carry on again and something had to change . As I previously alluded , this call of nature to change is louder for the bigger the establishment is . Look around what is happening in the world right now .
But to ‘change’ , the first reflex action of human beings is fighting against each other , somehow .
War and peace , of course , is always naturally cyclical .
I am currently witnessing numerous ‘in-house fightings’ within organisations, including GP practices.
Strange but also egregious.
Please keep sending your comments in .From the positive side , this most extraordinary phenomenon of a confrontation between our profession and the government could represent a good opportunity for the ‘change’ I mentioned above.
My view😑😎
Dr Julius Parker summaries the situation with admirable clarity
However he is wrong, it is no illusion, there are no limits to a GP’s workload and responsibilities
GP’s have failed to arrange their affairs in a sensible professional safe manner.
The article presents a detailed, extensively researched exposure , of the mass professional delusion, that the public should understand, and sympathise with this failure.
In retirement, I speak to many proper professionals, who behave in a professional manner, and can report they have no understanding or sympathy.
Failure is failure.
Just the extra time for cleaning and PPE and the safety and physical distancing in the waiting rooms. NORMAL is still far away. It is impossible in the hours we have in one day to do what we did before. Sadly, we have months to go, I think before NORMAL resumes. I hate the way it is now, just as much as my patients do, but that is life
The on-line services crashed at my own surgery three days ago——With the extra burden thrust upon an apparently overwhelmed practice it decided to put its feet up and have a cup of coffee and a fag——
The on-line services crashed at my own surgery three days ago——With the extra burden thrust upon an apparently overwhelmed practice it decided to put its feet up and have a cup of coffee and a fag——so it was closed for half a day on the pretext of training purposes while calls were diverted to 111
Just say “no”. It works.
John Graham Munro… please, please go find somewhere else to troll. I think we are all very familiar by now with your dissatisfaction with your own practice, given the amount of disparaging comments you make. As you said in another post recently…… stop moaning and do something about it……. I am sure another local practice would love to take over your care.
Yes it does John, but they don’t.
The majority of contributors are from the BMA or LMC, and their language, fear, unfair etc , is the language of victimhood. Yet these are supposedly all intelligent professional people.
There have been many many similar articles,perhaps the most striking, those by Professor Gerada detailing her work with GP’s having nervous breakdowns. All reinforce the narrative of victimhood.
It must therefore be asked, are these doctors seeking victimhood, do they feel comfortable in this role, and seek to perpetuate it. The professor never expands on this theme, identifying how many are architects of their own demise.
If our colleagues enjoy the victim role, saying “no” , will be the last thing on their mind
Thomas Robinson——–quite–the poor things——-oops—-sorry L.B.
What few realise – is that pre-pandemic – that service was ABNORMAL.