Are patients ‘shopping around’ the GP marketplace?


Pulse’s newest investigation revealed new data on the number of practices applying to close their patient list – a last throw of the dice before handing back their contract. As part of this series, Eliza Parr explores whether this has had an impact on patients ‘shopping around’
Two years ago, former health secretary Thérèse Coffey’s infamous plan for patient access sought to equip patients with information to help them make ‘informed choices’ about where to take up GP services.
This information included the publication of practice-level performance data showing the number of appointments delivered and waiting times.
So with the ever-growing political and media focus on access over recent years, and armed with new data to compare local practices, it might make sense to see a rise in patients moving around the marketplace.
But this type of ‘consumer’ behaviour among patients seems to have decreased significantly over the last five years.
In 2018, 36% of registrations for GP practices in England were for patients who had not also moved address at the same time, suggesting they moved for other reasons such as preference. This figure has dropped to 12% for the whole of 2022, and just 7.2% in the first quarter of 2023.
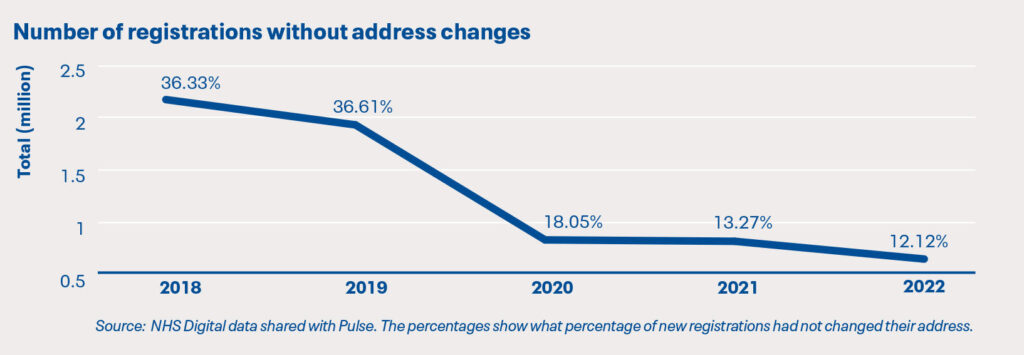
This downward trend could be linked to the uptick in practices formally closing their lists – if more practices are struggling to take on new patients, there may be fewer local options for patients to switch to.
Some patients in Merseyside have experienced just that. When one practice in the local area began to struggle maintaining access due to staffing issues, patients on their list became frustrated and wanted to move elsewhere. A GP partner at a neighbouring practice says they saw an influx of new patient applications which they struggled to ‘absorb’.
As a result, the GP partner and two other practices ‘coordinated’ an informal closure whereby patient applications were not accepted if they were already registered with a GP in the local area.
‘Patients felt they weren’t getting the service they wanted. I know there were some staff problems with that practice. So, using patient choice, they were coming to the other practices in the locality in large numbers that we couldn’t absorb in the timeframe.’
Capacity issues stopped these patients from exercising their right to choose a GP provider. The ability to ‘shop around’ seems to depend on adequate resourcing in neighbouring practices.
So if patients are shopping around less and less, what has Thérèse Coffey’s masterplan achieved? Publication of practice-level data over the last two years has provided easy fodder for news stories showing the ‘best’ and ‘worst’ practice in any given area, fuelling patient dissatisfaction.
Negative media narratives affect GP staff too – a study last year found that ‘inaccurate and unfair’ coverage of GPs in UK newspapers was worsening the GP workforce crisis. And recently, a local council report warned that GP practice staff face rising abuse due to media reporting.
Leicester, Leicestershire and Rutland (LLR) LMC chair Dr Grant Ingrams says the practice-level data isn’t useful because it doesn’t capture ‘why’ waiting times might be long.
‘They don’t tell you the wait’s so long because it’s an incredibly popular service, because they’ve got fantastic GPs, or because the practice has just had a GP leave and they can’t recruit…Sometimes there are things that the practice itself could do. But for a lot of practices, they are so distressed and frustrated because so much of this they have no control over.’
Without context, practice-level access figures may not be as helpful as Ms Coffey had planned. In fact, Dr Ingrams tells Pulse that even when patients do decide to look elsewhere, he has seen lots of them ultimately revert back to their original practice.
‘Over the years I’ve regularly seen patients who leave because they don’t like your service. They don’t feel it’s responsive enough or quick enough or whatever. And then, within six months or a year they come back, mainly because we’re their closest practice, and they’ve tried another practice and realised that it’s the same. Practices are all suffering similarly.’
With all practices under under capacity and cost pressures – and some feeling forced to close their list – patients seeking greener grass may struggle. But the significant reduction in this behaviour over recent years suggests the ability to shop around is not a priority for most patients.
Indeed, the most recent GP access plan makes no mention of patients making ‘informed choices’. Although monthly practice-level appointment data continues to be published, the Government’s interest in promoting a GP marketplace seems to have waned.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [2]
Please note, only GPs are permitted to add comments to articles











1) local patients around here may wish to, but often cannot due to distance to next GP surgery!
2) the reason for the higher numbers of patients changing GP without change of address in recent years could be due to surgery closures, branch surgery closures, and loss of bus services. In the last 2 years, they just cannot be bothered to access GPs at all.
In 1980’s practices wanted to have more patients because payment was based on capitation fee and basic practice allowance apart from items of service.. Changing a gp practice required 2 weeks notice when they will be asked again if they really wanted to change gp practice. How things have changed now. Choice of doctor depends on proximity of practice, easy access , good communication skill and good clinical acumen. Most important of all is how patient feels after consultation..