LMCs to hold special conference to discuss new GP contract
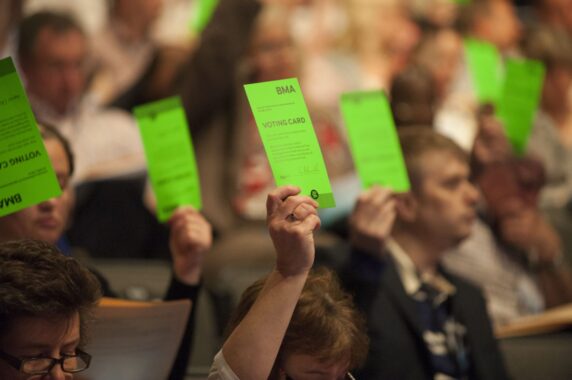
England’s LMCs will hold a special conference to discuss the new GP contract to be negotiated in 2024.
Ahead of the meeting, LMCs have been asked to consider what ‘is needed’ regarding ‘collective action/industrial action’ as well as ‘non-NHS options/Plan B’.
It comes as the BMA’s GP Committee last week held an emergency meeting to discuss the contract as well as current pressures and the ‘potential actions GPs can take’.
In a recent letter to GPs, England LMC conference chair Dr Shaba Nabi said that this year’s annual England LMC conference will span two days in November, with a ‘special conference’ to take place on the second.
She said: ‘The purpose of the special conference is to discuss a vision for English general practice with which to negotiate a new GP contract in 2024.’
She set out that while the first day will see motions submitted on key topics for debate such as workforce, workload and the PCN DES, as is usually the case at the LMC conference, the second day will have ‘discussions within break-out rooms, with a few key debates’.
Dr Nabi asked all LMCs to ‘prepare for these discussions’ by completing statements on the following questions:
- What does your LMC think is needed regarding GP contractual models?
- What does your LMC think is needed regarding general practice within the ICS?
- What does your LMC think is needed regarding non-NHS options/Plan B
- What does your LMC think is needed regarding collective action/industrial action options?
The conference is due to take place on Thursday 24 and Friday 25 November in London.
Meanwhile, the BMA’s GP Committee held an emergency meeting on Thursday last week to discuss both its ‘negotiating strategy’ for the coming year and what ‘actions’ GPs can themselves take.
Its latest email bulletin said the GPC met to ‘discuss our concerns about ongoing pressures in general practice and any potential actions that GPs can take as a profession in response to the underinvestment by the Government and the crippling workloads faced by GPs’.
It added: ‘The Committee also debated the GP contract, discussing what needs to be done to support practices struggling with inadequate premises, maintaining the declining workforce, bureaucracy and our negotiating strategy for the forthcoming year.’
GPC England representatives will provide reports from the meeting to their constituencies, it said.
In March, the BMA revealed what amendments it had requested – and NHS England had rejected – for the 2022/23 GP contract, including a ‘recovery fund’ for long-term conditions and changes to QOF and childhood immunisation payments.
It also revealed that it had begun talks around a new GP contract once the five-year deal concludes in 2024/25.
While the 2022/23 GP contract update was imposed without agreement from the BMA, the proposals could indicate the direction the new GPC leadership wants to take the GP contract in future negotiations.
GPs are currently bound to a five-year agreement which is due to expire on 31 March 2024, and the BMA had previously said it was not seeking to renegotiate the current five-year GP contract, outside of the usual annual amendments.
The ‘default’ position is for the existing contract to ‘automatically roll forward unless it is changed’ when the five-year framework concludes at the end of March 2024.
However, the BMA has told Pulse that it remains in the early stages of preparations for any GP industrial action.
Related Articles
READERS' COMMENTS [2]
Please note, only GPs are permitted to add comments to articles










I’d advocate the cancellation of both QOF and PCN+DES performance requirements, with all this funding rolled into core Practice funding.
We probably now take for granted the onerous burden of the annual recall system for ‘at risk’ groups.
No evaluation studies have demonstrated any value to patients. Practices might free up 10,000 appointments per year (for a 15,000 patient list), plus the admin, results etc which this system generates.
There’s no chance that NHSE will agree to this, but with appropriate leverage it might be possible to both free up thousands of appointments and to reclaim some autonomy on how we organise patient care in general practice.
We also need a new way to organise doctors’ representation as a profession. This might be most effective if all doctors were to affiliate toone body; it seems to me that primary and secondary care doctors have more in common than not and we would all benefit from such a collective voice.
Anyone going to whistleblowe this sold off system or just say it’s all ok?